If you are interested in products and services related to the research phase in this field, please contact for further inquiries.
Femoral neck fractures represent a significant clinical challenge, particularly in the aging population. These fractures often result from low-energy trauma, such as falls, and can lead to severe mobility issues and long-term disability. The femoral neck, a critical anatomical structure connecting the femoral head to the shaft of the femur, plays a vital role in hip joint stability and function. Disruption of this structure through fracture necessitates precise surgical intervention to restore function and minimize complications.
Screw fixation is a commonly employed surgical technique for treating femoral neck fractures. This method involves the insertion of screws into the femoral head and neck to stabilize the fracture and promote healing. While screw fixation can provide effective stabilization, it is not without its complications. One such complication is femoral neck shortening, which can occur postoperatively and significantly impact patient outcomes.
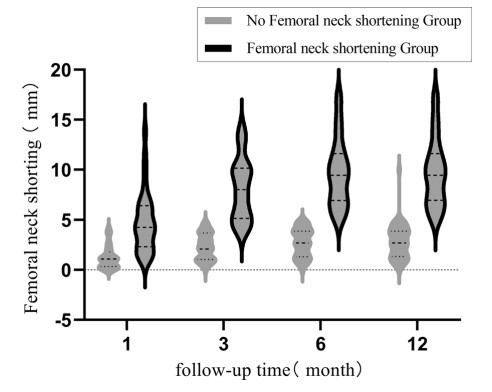 Fig.1 Comparison of femoral neck shortening between the two groups at postoperative follow-up. (Wang K., et al., 2023)
Fig.1 Comparison of femoral neck shortening between the two groups at postoperative follow-up. (Wang K., et al., 2023)
Incidence and Epidemiology of Femoral Neck Shortening
Recent studies have highlighted the prevalence of femoral neck shortening following screw fixation. Wang et al. (2023) reported an incidence rate of 39.1% in a cohort of 87 patients followed for over 12 months postoperatively. This rate is consistent with other studies, such as Stockton et al. (2015), who observed a 28% incidence of shortening in their case series. The incidence of severe shortening, defined as >10mm, was 17.2% in the study by Wang et al., indicating that a significant number of patients experience substantial shortening.
The epidemiology of femoral neck shortening is influenced by various factors, including patient demographics and fracture characteristics. Age, sex, and BMI did not show significant differences between patients with and without shortening in the study by Wang et al. However, fracture type and cortical comminution were significant predictors of shortening. These findings underscore the importance of understanding the underlying fracture morphology and patient-specific factors in predicting and managing femoral neck shortening.
Factors Influencing Femoral Neck Shortening
Cortical Comminution
Cortical comminution, or the fragmentation of the cortical bone at the fracture site, is a significant predictor of femoral neck shortening. Wang et al. (2023) found that cortical comminution was present in 82.4% of patients with shortening compared to 28.3% in those without shortening. This finding is supported by previous studies, such as Liu et al. (2013), who demonstrated that cortical comminution leads to increased micromovement and instability at the fracture site, contributing to shortening.
Fracture Type and Classification
Fracture type, as classified by the Garden and Pauwels systems, also plays a crucial role in predicting femoral neck shortening. Garden III and IV fractures, which are more displaced and complex, had a higher incidence of shortening compared to Garden I and II fractures. Pauwels classification, based on the angle of the fracture line, did not show a significant correlation with shortening in the study by Wang et al. However, the predominance of Pauwels type III fractures in their cohort suggests that shear forces and pressure loads at the fracture site may influence shortening.
Quality of Reduction
The quality of fracture reduction during surgery is another critical factor influencing femoral neck shortening. The study by Wang et al. utilized the Garden reduction alignment index to assess reduction quality, finding that poor reduction quality (levels III and IV) was significantly associated with shortening. Achieving anatomic reduction is essential to minimize postoperative complications and ensure optimal functional outcomes.
Clinical Implications and Functional Outcomes
- Impact on Hip Function
Femoral neck shortening can have a significant impact on hip function, as evidenced by lower hip Harris scores in patients with shortening. The hip Harris score, a comprehensive measure of hip function, includes pain level, functional status, deformity, and range of motion. Wang et al. (2023) reported a mean hip Harris score of 83.99 in the shortening group compared to 90.87 in the non-shortening group, indicating a substantial functional deficit in patients with shortening.
- Fracture Healing
Despite the functional impact of femoral neck shortening, the study found no significant difference in fracture healing rates between the shortening and non-shortening groups. Both groups exhibited high healing rates, suggesting that while shortening can impair function, it does not necessarily hinder the biological process of bone healing. This finding highlights the need to focus on minimizing shortening to preserve hip function, even though it may not affect healing.
Surgical Techniques and Postoperative Management
Surgical Method
The surgical technique employed in the study by Wang et al. involved precise placement of kerf pins and a threaded bone traction nail to correct displacement and rotation. The use of fluoroscopy ensured accurate guide pin placement, crucial for effective fixation. Achieving anatomic reduction and proper screw placement are essential steps in minimizing the risk of femoral neck shortening.
Postoperative Care
Postoperative care, including infection prevention, deep vein thrombosis prophylaxis, and gradual weight-bearing exercises, is critical in supporting fracture healing and functional recovery. Regular follow-up and imaging are essential to monitor for complications like shortening and adjust treatment plans accordingly. The study by Wang et al. emphasized the importance of careful postoperative management in optimizing patient outcomes.
Future Directions and Research
- Biomechanical Innovations
Future research should focus on developing and evaluating new biomechanical solutions to address cortical comminution and improve reduction quality. Innovative surgical techniques and implant designs could offer enhanced stability and minimize the risk of femoral neck shortening.
- Long-Term Follow-Up Studies
Long-term follow-up studies are necessary to assess the long-term functional outcomes and potential late complications like femoral head necrosis. Understanding the long-term impact of femoral neck shortening on patient quality of life and mobility will inform better surgical strategies and postoperative care.
- Patient-Specific Factors
Further exploration of patient-specific factors, such as bone quality and metabolic factors, could provide additional insights into the risk of femoral neck shortening. Personalized surgical approaches based on individual patient characteristics may improve outcomes and reduce complications.
Conclusion
The study by Wang et al. (2023) provides valuable insights into the incidence and influencing factors of femoral neck shortening after screw fixation. Cortical comminution, fracture type, and reduction quality are significant predictors of shortening. While femoral neck shortening does not significantly affect fracture healing, it can substantially impair hip function, emphasizing the need for strategies to minimize this complication. Future research should focus on developing innovative surgical techniques, conducting long-term follow-up studies, and exploring patient-specific factors to enhance treatment outcomes for femoral neck fractures.
If you have related needs, please feel free to contact us for more information or product support.
Reference
- Wang, Kai, et al. "Incidence and factors influencing neck shortening after screw fixation of femoral neck fractures with the femoral neck system." Journal of Orthopaedic Surgery and Research 18.1 (2023): 317.
This article is for research use only. Do not use in any diagnostic or therapeutic application.



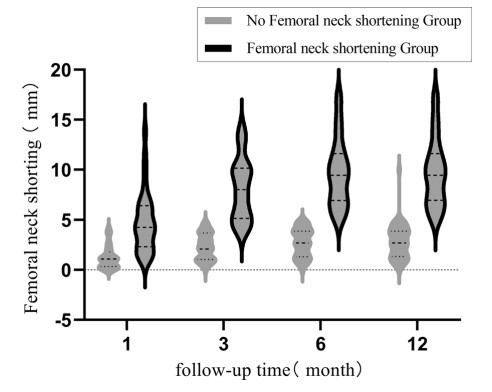 Fig.1 Comparison of femoral neck shortening between the two groups at postoperative follow-up. (Wang K., et al., 2023)
Fig.1 Comparison of femoral neck shortening between the two groups at postoperative follow-up. (Wang K., et al., 2023)