If you are interested in products and services related to the research phase in this field, please contact for further inquiries.
Non-invasive blood glucose monitoring has emerged as a pivotal area of research in the medical technology sector, driven by the increasing prevalence of diabetes worldwide. Traditional invasive methods, while effective, are often associated with discomfort and potential risks, leading to a significant need for non-invasive alternatives. This comprehensive review explores the latest advancements in non-invasive blood glucose monitoring technologies, focusing on optical, microwave, and electrochemical methods, and highlights the challenges and future prospects in this field.
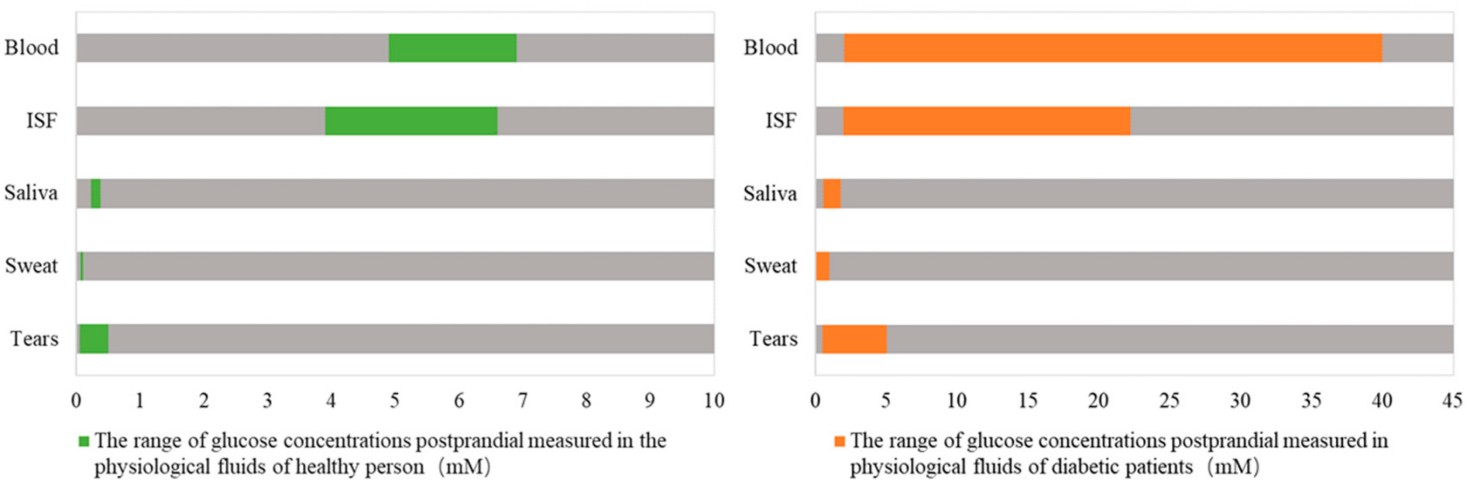 Fig.1 Contrast of glucose concentrations in different physiological fluids between healthy and diabetic people. (Tang L., et al., 2020)
Fig.1 Contrast of glucose concentrations in different physiological fluids between healthy and diabetic people. (Tang L., et al., 2020)
Optical Methods: A Spectrum of Possibilities
Optical methods for non-invasive glucose monitoring leverage light to detect glucose levels in the body. These methods include near-infrared (NIR) and mid-infrared (MIR) spectroscopy, optical polarimetry, Raman spectroscopy, and fluorescence.
Near-Infrared (NIR) and Mid-Infrared (MIR) Spectroscopy
NIR and MIR spectroscopy are based on the absorption of light by glucose molecules. NIR light, with a wavelength range of 680–2500 nm, can penetrate deeper into tissues, making it suitable for continuous monitoring. However, the presence of water and other molecules in tissues can interfere with the readings. MIR light, with a wavelength range of 2500–25,000 nm, offers higher specificity for glucose but is limited by its weaker penetration depth.
Recent advancements in NIR spectroscopy include the development of multivariate calibration models that use algorithms to improve the accuracy of glucose readings. For instance, Xue et al. demonstrated a model with a root mean square error of validation (RMSEP) of 0.061 and a correlation coefficient of 99.33%. These improvements highlight the potential of NIR spectroscopy for non-invasive glucose monitoring.
Optical Polarimetry (OP)

Optical polarimetry relies on the optical rotation of polarized light when it passes through a glucose solution. Glucose molecules cause a rotation of the polarized plane, which is proportional to the glucose concentration. This method is simple and non-invasive, but faces challenges due to the scattering properties of human tissues and the presence of other optically active molecules.
Malik et al. proposed a dual-wavelength polarization technique that uses multiple linear regression (MLR) to reduce errors and improve accuracy. This method showed a mean error of 22.4 mg/dL and a linear correlation coefficient of 0.996. However, further research is needed to validate these findings in clinical settings.
Raman Spectroscopy
Raman spectroscopy detects glucose by analyzing the scattered light produced when a laser interacts with glucose molecules. This method offers high specificity due to the unique vibrational modes of glucose. However, the weak Raman signals and interference from background noise pose significant challenges.
Recent studies have shown that surface-enhanced Raman spectroscopy (SERS) can amplify the weak signals, making it a promising technique for non-invasive glucose monitoring. For example, Yang et al. demonstrated a SERS-based sensor that achieved a detection error range within 0.5 mM, suitable for monitoring physiological glucose levels.
Fluorescence Method
Fluorescence-based sensors detect glucose by measuring the changes in fluorescence intensity when glucose interacts with specific fluorophores. Quantum dots (QDs) and carbon dots (CDs) are commonly used as fluorescent probes due to their high sensitivity and specificity.
Zhai et al. developed a fluorescence ratiometric sensor using CDs and m-dihydroxybenzene (mDHB) oxides, which showed a linear relationship between glucose concentration and fluorescence ratio. This method achieved a detection limit of 0.35 mM, demonstrating its potential for non-invasive glucose monitoring.
Microwave Methods: Penetrating the Surface
Microwave methods for non-invasive glucose monitoring utilize the interaction between electromagnetic waves and biological tissues. Microwaves can penetrate tissues and provide information about the dielectric properties of the tissue, which are influenced by glucose levels.
- High-Sensitivity Microwave Biosensors
Recent advancements in microwave technology have led to the development of high-sensitivity biosensors that can detect glucose levels with high accuracy. For example, Kumar et al. designed a microwave biosensor with a low resonance frequency of 1.50 GHz and a high sensitivity of 117.5 MHz/mg/mL. This sensor exhibited a linear response with a correlation coefficient of 0.9987, making it a promising candidate for non-invasive glucose monitoring.
Electrochemical Methods: Harnessing Biofluids
Electrochemical methods for non-invasive glucose monitoring involve the measurement of glucose levels in biofluids such as saliva, tears, sweat, and interstitial fluid (ISF). These methods leverage the correlation between glucose levels in these fluids and blood glucose levels.
Reverse Iontophoresis (RI) Technology
Reverse iontophoresis is a technique that uses an electric current to extract glucose from the skin's ISF. The GlucoWatch, a pioneering device using RI technology, demonstrated the potential of this method for non-invasive glucose monitoring. However, limitations such as the need for calibration and skin irritation have hindered its widespread adoption.
Recent advancements in RI technology include the use of microneedle arrays to enhance the extraction of ISF. Zhu et al. developed a dissolving gelatin methacryloyl (GelMA) microneedle patch that efficiently extracted ISF and quantified glucose levels. This method showed a linear correlation between detected glucose concentrations and actual concentrations, highlighting its potential for non-invasive monitoring.
Future Directions and Challenges
The development of non-invasive blood glucose monitoring technologies faces several challenges, including improving sensitivity, reducing measurement delays, and ensuring patient comfort. Future research should focus on integrating multiple physical parameters and biomarkers to enhance the accuracy and reliability of non-invasive methods.
The integration of wearable devices with non-invasive sensors holds great promise for continuous glucose monitoring. Advances in nanotechnology, materials science, and computational algorithms will play a crucial role in overcoming current limitations and developing robust, user-friendly devices.
Conclusion
Non-invasive blood glucose monitoring represents a significant leap forward in diabetes management. While current methods offer promising results, further research and development are needed to address existing challenges and bring these technologies to the market. The ultimate goal is to provide patients with a painless, accurate, and convenient alternative to invasive methods, thereby improving their quality of life and health outcomes. As research continues to advance, the future of non-invasive glucose monitoring looks increasingly bright, offering hope to millions of people living with diabetes.
If you have related needs, please feel free to contact us for more information or product support.
Reference
- Tang, Liu, et al. "Non-invasive blood glucose monitoring technology: a review." Sensors 20.23 (2020): 6925.
This article is for research use only. Do not use in any diagnostic or therapeutic application.



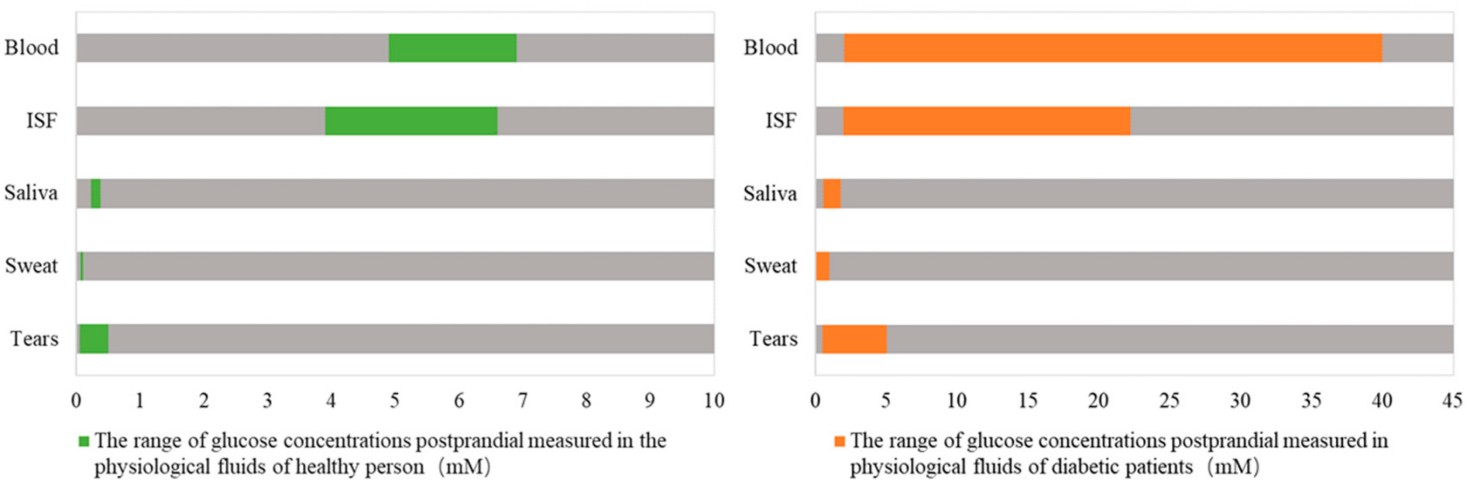 Fig.1 Contrast of glucose concentrations in different physiological fluids between healthy and diabetic people. (Tang L., et al., 2020)
Fig.1 Contrast of glucose concentrations in different physiological fluids between healthy and diabetic people. (Tang L., et al., 2020)