If you are interested in products and services related to the research phase in this field, please contact for further inquiries.
Smart bandages represent a significant leap forward in the integration of wearable technology and healthcare. These advanced medical devices combine traditional wound care with sophisticated electronic sensors, offering real-time monitoring and treatment capabilities. The evolution of bandages from simple wound coverings to intelligent, interactive devices underscores a broader trend in healthcare technology: the move towards personalized, continuous, and non-invasive care. This article explores the scientific and technological advancements that have made smart bandages possible, their current applications, and the potential future developments that could revolutionize wound care and beyond.
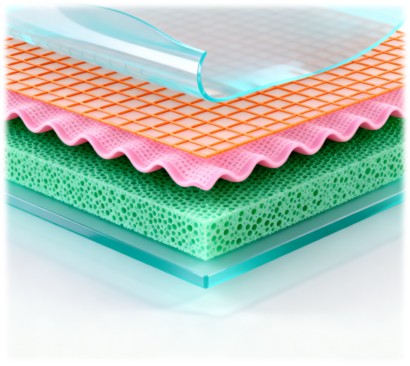
 Fig.1 Schematic illustration of the smart bandage structure levels. (Levin A., et al., 2023)
Fig.1 Schematic illustration of the smart bandage structure levels. (Levin A., et al., 2023)
Historical Context and Evolution
The journey of bandages from ancient times to the present day is a testament to human ingenuity and the relentless pursuit of better healthcare solutions. Early bandages, such as those used in Ancient Egypt, were primarily made of linen and served to cover wounds and prevent infection. The use of natural disinfectants like wine, vinegar, and honey was common. The Homeric poems, written around 800 B.C., described over 130 types of wounds, highlighting the complexity and variety of injuries treated during that era.
Significant advancements in bandage technology occurred during the 19th and 20th centuries, driven by the need for better wound management during wars. The introduction of sterilization techniques by Johnson & Johnson in the 19th century marked a major milestone, significantly reducing the risk of infection. The 20th century saw further innovations, such as the development of moist wound healing theory by Prof. George D. Winter in 1962, which emphasized the importance of maintaining a moist environment for optimal healing.
Modern Bandage Design and Functionality
Today's bandages are designed based on the four stages of wound healing: hemostasis, anti-inflammation, proliferation, and remodeling. These stages overlap and occur in a specific order, influenced by factors such as wound type, patient physiology, and the surrounding environment. Bandages are typically multi-layered, with each layer serving a specific function:
- Layer A: The delivery method, often made of paper or plastic, helps maintain the bandage's form until application.
- Layer B: The backing layer, made of materials like polypropylene or PET, provides structural support and acts as a barrier against fluids and microorganisms.
- Layer C: The adhesive layer, often made of silicon or acrylate, ensures the bandage adheres to the skin.
- Layer D: The absorbent layer, which can be made of cloth or foam, absorbs excess fluids and impurities.
- Layer E: The release liner, made of materials like poly-olefin-coated paper or PET, protects the adhesive surface before application.
Different types of bandages, such as gauzes, foam, hydrogel, hydrocolloid, and transparent films, offer varying levels of absorption, adherence, and protection. Each type is tailored to specific wound characteristics and healing requirements.
Functional Bandages: The Next Step in Evolution
The next step in bandage evolution was the introduction of functional properties to aid the healing process. Medicated bandages can be categorized into two groups:
- Symptomatic Treatment Bandages: These release anti-inflammatory, pain-relief, and anti-bacterial agents directly onto the wound.
- Bio-Active Bandages: These enhance tissue regeneration and the body's natural healing processes, often using materials like alginate, collagen, and chitosan.
These advancements laid the groundwork for the development of smart bandages, which integrate electronic sensors to monitor and respond to the healing process in real-time.
The Rise of Smart Wearable Bandages
The wearable technology market has grown exponentially, with devices ranging from smartwatches to fitness trackers. However, these devices often suffer from issues like poor adhesion to the skin, leading to inaccurate readings and user discomfort. Smart bandages, on the other hand, leverage the conformal contact and breathability of traditional bandages to provide a more reliable and comfortable platform for wearable sensors.
Smart bandages can be categorized into two main types based on their functionality:
- Passive Smart Bandages: These collect and transmit data to a user or healthcare provider. They can measure biophysical parameters like temperature, pressure, and motion, or biochemical parameters like pH and glucose levels.
- Active Smart Bandages: These not only collect data but also deliver treatments, such as drug delivery or electrical stimulation, in response to specific stimuli.
Passive Smart Bandages: Monitoring Health Parameters
Passive smart bandages are designed to monitor various health parameters without active intervention. They can be used for applications like fitness tracking, continuous health monitoring, and early detection of medical conditions. For example, a thin film bandage can be used as a strain sensor to monitor body movements, while hydrogel-based bandages can detect biochemical changes in sweat or wound exudate.
The development of passive smart bandages involves optimizing the properties of each layer to ensure maximum data quality. For instance, a bandage designed for heart rate monitoring might require a thicker adhesive layer for better adhesion and a more flexible backing layer for comfort. The choice of materials and fabrication methods, such as 3D printing or laser printing, also plays a crucial role in the performance and scalability of these devices.
Active Smart Bandages: Delivering Treatments
Active smart bandages take the concept of wearable biosensors a step further by integrating drug delivery systems and electrical stimulation capabilities. These bandages can respond to external stimuli like light, temperature, or pH, or receive direct commands from a control system. For example, a UV-responsive hydrogel bandage can release anti-bacterial agents upon exposure to UV light, while a bandage with microneedles can deliver drugs directly into the skin.
The development of active smart bandages requires a more complex architecture, combining multiple layers and functionalities into a single device. This includes integrating sensors, drug reservoirs, microneedles, and electronic circuits into a flexible and conformal bandage. The goal is to create a multi-purpose platform that can monitor health parameters, deliver treatments, and provide real-time feedback to healthcare providers.
Manufacturing and Market Considerations
Introducing new products into a competitive market requires careful consideration of scalability, cost, and regulatory approval. Using existing bandage materials and manufacturing processes can mitigate many of these risks. For example, leveraging raw materials from established manufacturers like 3M or Johnson & Johnson can simplify the testing and certification process, ensuring faster market entry.
Another approach is to partner with converters, companies that specialize in further processing raw materials into final products. This strategy is particularly useful for small-scale production or when manufacturing facilities are not available locally. Converters can help adapt existing materials to new applications, ensuring that the final product meets the desired specifications.
Emerging technologies like 3D printing and electrospinning offer new possibilities for bandage manufacturing. 3D printing allows for the direct deposition of both the bandage and electronic components onto the skin, creating a seamless and customizable product. Electrospinning, on the other hand, can produce nanofibrous dressings with unique properties, such as enhanced absorption and drug delivery capabilities.
Future Perspectives and Potential Applications
The future of wearable technology lies in the seamless integration of sensors, electronics, and materials science to create devices that are not only functional but also comfortable and user-friendly. Smart bandages, with their ability to monitor and treat wounds in real-time, represent a significant step towards this goal. They have the potential to revolutionize healthcare by providing continuous, non-invasive monitoring and personalized treatment options.
Imagine a future where a smart bandage can detect a physiological disorder and automatically contact a healthcare provider, or where a bandage can deliver medication and monitor its effectiveness in real-time. These advancements could lead to better patient outcomes, reduced healthcare costs, and improved quality of life for individuals with chronic conditions.
Conclusion
The journey from traditional bandages to smart wearable biosensors is a testament to human ingenuity and the relentless pursuit of better healthcare solutions. By leveraging the knowledge and manufacturing practices accumulated over centuries, we can accelerate the development and adoption of smart bandages. The future of wearable technology is bright, and with continued advancements in materials, electronics, and artificial intelligence, smart bandages could become an essential part of everyday life, transforming how we monitor and manage our health.
If you have related needs, please feel free to contact us for more information or product support.
Reference
- Levin, Arie, Shu Gong, and Wenlong Cheng. "Wearable smart bandage-based bio-sensors." Biosensors 13.4 (2023): 462.
This article is for research use only. Do not use in any diagnostic or therapeutic application.
Bandage Accessories Series



 Fig.1 Schematic illustration of the smart bandage structure levels. (Levin A., et al., 2023)
Fig.1 Schematic illustration of the smart bandage structure levels. (Levin A., et al., 2023)