- Home
- Resource
- Disease Diagnosis
- Autoimmune Diseases
- The Diagnostic Landscape of Autoimmune Hepatitis (AIH) From Serology to Histology
- Home
- IVD
- By Technology Types
- By Diseases Types
- By Product Types
- Research
- Resource
- Distributors
- Company
Autoimmune hepatitis (AIH) is a chronic inflammatory liver disorder whose diagnosis demands a meticulous synthesis of clinical, serological, and histological findings. No single test is sufficient; instead, confirmation relies on integrating elevated immunoglobulin G (IgG) levels, characteristic autoantibody profiles, and distinctive histopathological features while excluding other liver diseases. This resource provides a comprehensive overview of the AIH diagnostic pathway, from initial clinical suspicion to advanced serological testing and gold-standard histological verification.
Autoimmune hepatitis (AIH) is a chronic inflammatory liver disease characterized by the immune system mistakenly attacking hepatocytes, leading to progressive liver damage, fibrosis, and potential cirrhosis if untreated. Its diagnosis hinges on a multifaceted approach, integrating clinical presentation, characteristic serological biomarkers, and definitive histological findings while rigorously excluding other liver diseases. This synthesis of clinical, laboratory, and pathological evidence is essential for accurate diagnosis and timely intervention.
 Fig.1 Algorithm for the diagnosis of autoimmune hepatitis (AIH) in adults. (Mercado L A, et al., 2024)
Fig.1 Algorithm for the diagnosis of autoimmune hepatitis (AIH) in adults. (Mercado L A, et al., 2024)
Clinical suspicion for autoimmune hepatitis (AIH) arises from a combination of non-specific symptoms, biochemical evidence of liver inflammation, and exclusion of other common etiologies. Key indicators include unexplained fatigue, jaundice, arthralgia, or elevated liver transaminases (AST/ALT) disproportionate to alkaline phosphatase, often accompanied by hypergammaglobulinemia, particularly elevated immunoglobulin G (IgG). This suspicion should prompt further serological and histological investigation, especially when viral, alcoholic, metabolic, or drug-induced liver diseases have been ruled out.
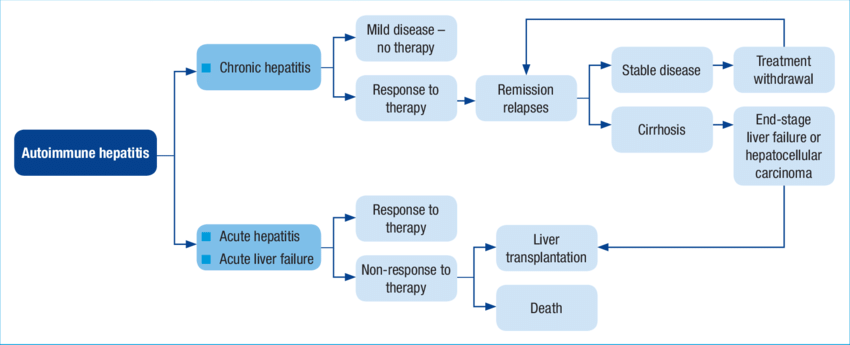 Fig.2 Clinical presentation and course of autoimmune hepatitis (AIH). (Theocharidou E, Heneghan M A., 2018)
Fig.2 Clinical presentation and course of autoimmune hepatitis (AIH). (Theocharidou E, Heneghan M A., 2018)
Serological testing forms the cornerstone of the initial diagnostic workup for autoimmune hepatitis (AIH). It provides critical immunological evidence to support the diagnosis, aid in classification, and differentiate AIH from other liver diseases. The primary goal of serology is to detect circulating autoantibodies directed against the patient's own hepatocytes. The pattern and specificity of these antibodies are key to understanding the disease.

Considered the traditional gold standard, IIF is a highly sensitive technique that detects autoantibodies by visualizing their unique staining patterns on tissue-specific substrates, but it requires significant expertise to interpret.
These automated, objective solid-phase assays offer high throughput and excellent specificity by detecting antibodies bound to purified recombinant or purified antigens, making them ideal for screening and confirmation.
It allows for the simultaneous detection of multiple autoantibodies from a single patient sample by probing serum against a panel of discrete antigens immobilized on a solid strip, providing a comprehensive and efficient diagnostic profile.
Liver biopsy and subsequent histological examination remain the cornerstone and gold standard for confirming a diagnosis of autoimmune hepatitis (AIH). While serology provides crucial immunological clues, histology offers an unparalleled view of the actual architectural damage and inflammatory activity within the liver, allowing for definitive diagnosis, staging of disease severity, and exclusion of other conditions. It is particularly indispensable in cases of seronegative AIH (where autoantibodies are absent) and for assessing the degree of fibrosis, which critically guides treatment decisions and prognosis. The main histopathological features are as follows:

The future of autoimmune hepatitis (AIH) diagnostics is poised to move beyond reliance on traditional autoantibodies and liver biopsy towards a more integrated, precision-based approach. This evolution will be driven by the discovery and validation of novel serological biomarkers (e.g., anti-SLA/LP, anti-F-actin) and the adoption of advanced technologies like multiplex immunoassays and artificial intelligence for pattern recognition in histology. These innovations aim to enhance diagnostic accuracy, particularly in seronegative cases, enable earlier detection through improved risk stratification, and ultimately guide more personalized treatment strategies tailored to individual patient profiles and disease mechanisms.
To support effective autoimmune hepatitis (AIH) management, Alta DiagnoTech offers a comprehensive and precise IVD product line, including immunoassay kits for key serological markers such as ANA, F-actin-specific ASMA, anti-LKM1, and anti-SLA/LP, quantitative IgG assay kits, and more. If you have related needs, please feel free to contact us for more information or product support.
References
| Cat.No | Product Name | Price |
|---|---|---|
| EK-YJL-0093 | Human Anti-nuclear Antibody, ANA ELISA Kit | Add To Cart |
| EK-YJL-0078 | Mouse Anti-nuclear Antibody (IgG) ELISA Kit | Add To Cart |
| EK-YJL-1659 | Mouse Anti-Smooth Muscle Antibody, ASMA ELISA Kit | Add To Cart |
| EK-YJL-1719 | Human Anti-smooth Muscle Antibody, ASMA ELISA Kit | Add To Cart |
| IP-00193 | Adenovirus, RSV and Influenza A+B combo rapid assay kit | Add To Cart |
| EC-0031 | Human IL-1 beta ELISA Kit | Add To Cart |
| CA-00154 | Chikungunya IgG/IgM rapid assay kit | Add To Cart |
| EC-0079 | Human IL-8 ELISA kit | Add To Cart |
| EC-0080 | Human IL-10 ELISA kit | Add To Cart |
| CA-00159 | Zika IgG/IgM rapid assay kit | Add To Cart |
| EC-0016 | Murine IL-15 ELISA Kit | Add To Cart |
| EC-0034 | Human IL-13 ELISA Kit | Add To Cart |
| CA-00179 | Mycoplasma pneumoniae IgM rapid assay kit | Add To Cart |
| EC-0059 | Human trail R1 ELISA Kit | Add To Cart |
| EC-0052 | Human CD95 ELISA Kit | Add To Cart |
This article is for research use only. Do not use in any diagnostic or therapeutic application.
|
There is no product in your cart. |