- Home
- Resource
- Explore & Learn
- Preanalytical Errors in Hematology Laboratories
- Home
- IVD
- By Technology Types
- By Diseases Types
- By Product Types
- Research
- Resource
- Distributors
- Company
Hematology laboratories are the backbone of modern diagnostic medicine, providing critical information on blood and its components that guide clinical decision-making. Despite technological advancements and stringent quality control measures, preanalytical errors remain a persistent challenge. These errors, occurring before the actual testing of samples, can significantly impact the accuracy and reliability of test results, leading to misdiagnosis, inappropriate treatment, and increased healthcare costs. This article delves into the hidden challenges of preanalytical errors in hematology laboratories, exploring their types, frequencies, impacts, and strategies for mitigation.
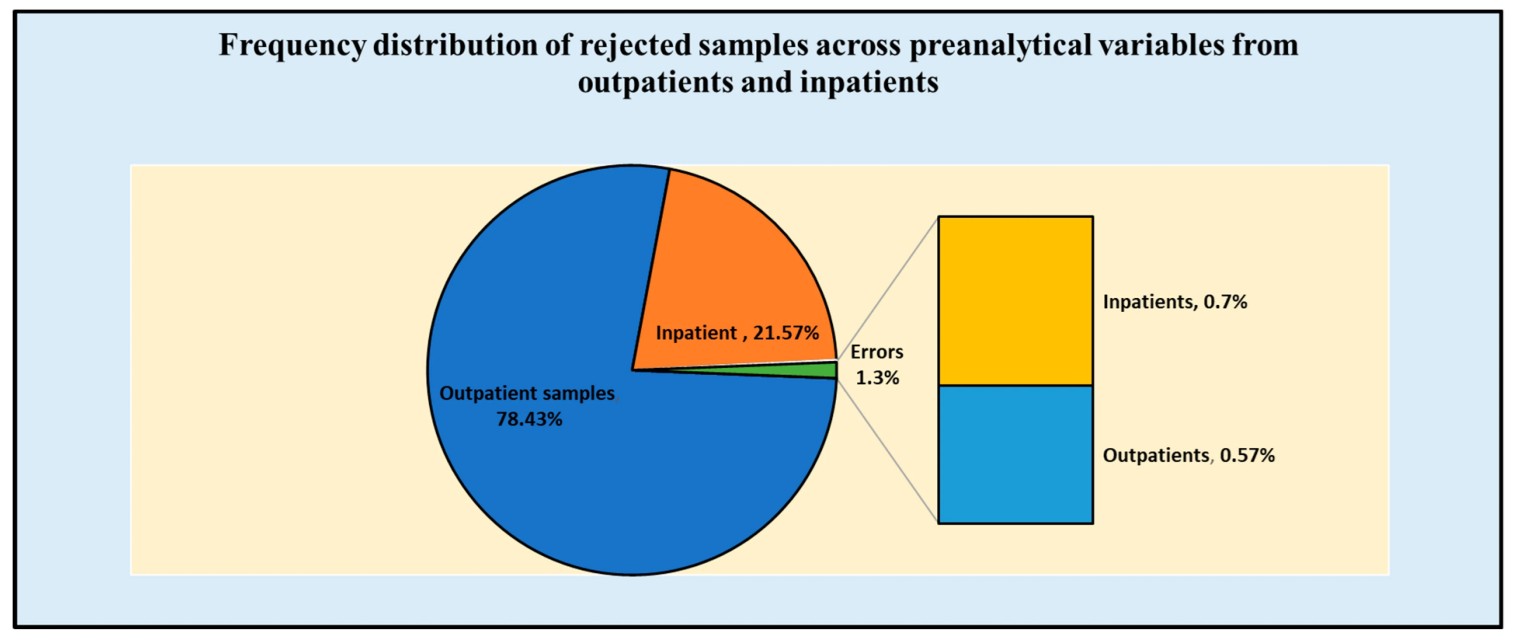 Fig.1 Frequency distribution of rejected samples across preanalytical variables from outpatients and inpatients. (Iqbal M. S., et al., 2023)
Fig.1 Frequency distribution of rejected samples across preanalytical variables from outpatients and inpatients. (Iqbal M. S., et al., 2023)

Insufficient Sample Volume
One of the most frequent preanalytical errors encountered in clinical settings is the collection of an insufficient blood sample. This issue can arise due to various factors, including improper venipuncture technique, small vein size, or premature withdrawal of the needle. Insufficient samples can lead to inaccurate test results, particularly for tests that require precise blood-to-anticoagulant ratios, such as coagulation studies. In these cases, inadequate sample volume can result in unreliable measurements, potentially delaying diagnosis and treatment.
Clotted Samples
Clotting of blood samples is another common preanalytical issue, often resulting from inadequate mixing of the sample with anticoagulant or delays in processing. When blood clots, it forms a solid mass that makes the sample unsuitable for analysis. This necessitates recollection of the sample, causing delays in diagnosis and increasing the burden on both healthcare providers and patients. Proper mixing and timely processing are essential to prevent clotting and ensure the integrity of the sample.

Hemolyzed Samples
Hemolysis, the rupture of red blood cells, is a significant preanalytical error that can occur due to rough handling of the sample, improper needle size, or prolonged storage before processing. Hemolyzed samples release cellular contents into the plasma, which can interfere with various hematological tests, leading to inaccurate results. This interference can affect the measurement of critical parameters such as hemoglobin levels and enzyme activities, potentially misleading clinical decisions. Proper handling and timely processing are crucial to minimize hemolysis and ensure accurate test results.

Incorrect Labeling and Identification
Errors in patient identification and sample labeling can have severe consequences, including misdiagnosis and incorrect treatment. These critical errors often stem from human factors, such as fatigue, distraction, or lack of training. Incorrect labeling can lead to the wrong patient receiving test results, causing unnecessary anxiety and potentially harmful interventions. Ensuring accurate patient identification and sample labeling is essential to maintain the reliability and safety of diagnostic processes. Implementing standardized protocols and double-checking procedures can help mitigate these risks and ensure that each sample is correctly associated with the appropriate patient.
Lack of Training
Inadequate training of phlebotomists and laboratory personnel in proper sample collection and handling techniques is a significant contributor to preanalytical errors. Continuous education and certification programs can help mitigate this risk.
Fatigue and Distraction
High workload and long hours can lead to fatigue and distraction among laboratory staff, increasing the likelihood of errors. Implementing ergonomic practices and providing regular breaks can help alleviate these issues.
Inadequate Standardization
Lack of standardized procedures for sample collection, handling, and transportation can introduce variability and errors. Developing and enforcing standardized protocols can help ensure consistency and accuracy.
Poor Communication
Effective communication between laboratory personnel, healthcare providers, and patients is crucial for minimizing preanalytical errors. Miscommunication can lead to incorrect sample collection, handling, or testing. Implementing clear communication channels and protocols can help mitigate this risk.
Preanalytical errors in hematology laboratories represent a significant challenge, impacting patient care, healthcare costs, and patient satisfaction. Understanding the types, frequencies, and causes of these errors is crucial for developing effective mitigation strategies. By standardizing procedures, providing regular training, leveraging technology, and implementing quality assurance programs, laboratories can significantly reduce preanalytical errors and improve the overall quality of healthcare services. As the healthcare landscape continues to evolve, a commitment to continuous improvement and patient-centered care will be essential in addressing this hidden yet critical issue.
If you have related needs, please feel free to contact us for more information or product support.
Reference
| Cat.No | Product Name | Price |
|---|---|---|
| HT-QCY-0003 | A, B & RhD Blood Type Test Kit | Add To Cart |
| HT-QCY-0009 | Sickle Cell Test Kit | Add To Cart |
| HT-QCY-0008 | Coagulation Function Analysis Kit | Add To Cart |
| HT-QCY-0007 | Coagulation Test Kit | Add To Cart |
| HT-QCY-0001 | Erythropoietin (EPO) Quantikine Test Kit | Add To Cart |
| HT-QCY-0002 | ABO & RhD Blood Type Test Kit | Add To Cart |
| HT-QCY-0010 | Anemia Test Kit | Add To Cart |
| HT-QCY-0005 | Single-use Blood Type Test Kit | Add To Cart |
| HT-QCY-0006 | Professional Coagulation Rapid Test Kit | Add To Cart |
| HT-QCY-0011 | Ferritin Test Kit | Add To Cart |
| HT-QCY-0004 | RhD Blood Type Test Kit | Add To Cart |
This article is for research use only. Do not use in any diagnostic or therapeutic application.
|
There is no product in your cart. |