Innovative Point-Of-Care Hematology Analysis
Hematology testing, encompassing the complete blood count (CBC) and differential white blood cell (WBC) counts, is a cornerstone of modern medical diagnostics. These tests are essential for diagnosing, monitoring, and guiding the treatment of numerous conditions, ranging from anemia and infections to leukemia and other hematologic malignancies. Traditionally, these tests have been performed in centralized laboratories, requiring specialized equipment and trained personnel. However, this model has inherent limitations, including delayed turnaround times (TAT), which can impact clinical decision-making and patient outcomes.
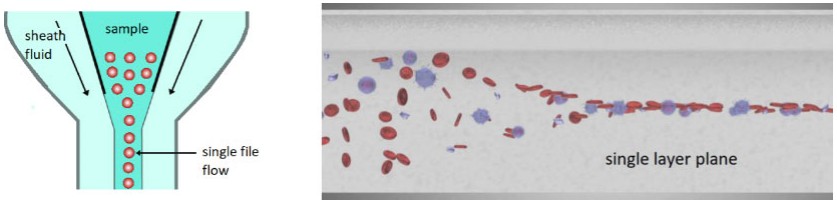 Fig.1 Standard hydrodynamic focusing technique (left) vs viscoelastic focusing (right). (Bransky A., et al., 2021)
Fig.1 Standard hydrodynamic focusing technique (left) vs viscoelastic focusing (right). (Bransky A., et al., 2021)
The Need for Point-of-Care (POC) Hematology Testing

Enhancing Patient Care Through Rapid Diagnostics
The escalating demand for point-of-care (POC) testing reflects a pressing need for swift, accessible diagnostic solutions that can be executed right at the patient's side. POC hematology testing, in particular, has the potential to markedly enhance patient care by delivering immediate results. This rapid data availability empowers clinicians to make timely decisions, thereby reducing the risk of adverse events and bolstering overall treatment efficacy. In high-stakes settings such as emergency departments (EDs) and intensive care units (ICUs), where time is of the essence, instant diagnostic information can be a critical determinant of patient outcomes. Moreover, in remote or underserved areas where access to centralized laboratories is limited, POC testing can bridge the gap, ensuring that patients receive prompt and appropriate care.

Overcoming Limitations of Centralized Laboratories
Despite being equipped with advanced instrumentation and staffed by highly trained professionals, centralized laboratories often encounter challenges that can delay the turnaround time (TAT) for test results. Issues such as sample transportation logistics, processing delays due to high sample volumes, and the need for specialized staff to operate complex equipment can all contribute to extended TATs. These delays are particularly detrimental in high-pressure environments like EDs, ICUs, and remote or underserved regions where timely access to diagnostic information is crucial. POC testing addresses these challenges by bringing diagnostic capabilities directly to the patient, thereby streamlining the healthcare delivery process. By eliminating the need for sample transportation and reducing reliance on centralized laboratory processing, POC testing ensures that patients receive timely and appropriate care, regardless of their location.
The HemoScreen: A Paradigm Shift in Hematology Testing
- Introduction to the HemoScreen Analyzer
The HemoScreen, developed by PixCell Medical Technologies, represents a significant breakthrough in point-of-care (POC) hematology testing. This compact and easy-to-use instrument integrates advanced flow cytometry and digital imaging technologies into a single, portable platform, delivering laboratory-equivalent performance directly at the patient's bedside. By combining these sophisticated techniques, the HemoScreen provides rapid, accurate, and comprehensive blood analysis, enabling healthcare providers to make informed decisions in real-time. The device's user-friendly design and rapid results make it particularly valuable in emergency departments, intensive care units, and remote settings where immediate access to diagnostic information is critical. The HemoScreen has received FDA clearance for POC use, marking a milestone in the evolution of hematology diagnostics and setting a new standard for rapid, reliable, and accessible blood testing.
- Technological Innovations Behind the HemoScreen
Microfluidic Viscoelastic Focusing (VEF)
At the heart of the HemoScreen's technology lies microfluidic viscoelastic focusing (VEF). This unique physical phenomenon occurs in microfluidic chambers filled with non-Newtonian fluids. As particles (or cells) flow through the chamber, they migrate toward the center, forming a sharply focused layer. This process, known as lateral migration, eliminates the need for complex hydrodynamic focusing techniques and sheath fluids, simplifying the design and operation of the analyzer.
Lab-on-a-Cartridge Design
The HemoScreen employs a disposable cartridge system, where each cartridge contains all necessary reagents and is factory-calibrated. This design ensures that the analyzer does not come into direct contact with the sample or reagents, minimizing maintenance requirements and reducing the risk of contamination. The cartridge automatically prepares the sample for analysis, replicating laboratory protocols in a streamlined manner.
Machine Vision and Artificial Intelligence (AI)
Unlike traditional hematology analyzers that rely on laser scattering or impedance measurements, the HemoScreen utilizes machine vision (digital image processing and analysis) combined with AI algorithms. This approach enables the analyzer to capture and analyze thousands of images of flowing cells on-the-fly, extracting hundreds of features from each cell. The AI algorithms then classify the cells based on their morphological and staining characteristics, providing accurate and reliable results.
- Clinical Performance and Validation
Numerous clinical studies have consistently demonstrated the HemoScreen's remarkable laboratory-equivalent performance across a diverse range of healthcare settings, including primary care clinics, oncology wards, intensive care units (ICUs), and operating rooms (ORs). These comprehensive evaluations have established the HemoScreen as a reliable and accurate diagnostic tool, capable of delivering results that closely match those of established laboratory analyzers. Specifically, studies have revealed high correlation coefficients between the HemoScreen and leading laboratory hematology analyzers such as the Sysmex XN series and the Abbott CellDyn Sapphire. For key parameters like mean cell volume (MCV), mean cell hemoglobin (MCH), and platelet count (PLT), the HemoScreen has shown exceptional agreement with these gold-standard devices, ensuring that healthcare providers can rely on its results for critical decision-making in various clinical contexts.
Advantages of the HemoScreen in Clinical Settings
- Improved Workflow and Efficiency
The HemoScreen's compact size and ease of use make it ideal for integration into various clinical settings, including emergency departments, intensive care units, and primary care clinics. Its rapid turnaround time (TAT), often less than 10 minutes, significantly reduces the time required for diagnostic testing. This allows clinicians to make faster decisions and initiate appropriate treatment promptly, thereby improving workflow efficiency. By streamlining the diagnostic process, the HemoScreen can lead to better patient outcomes and enhanced overall healthcare delivery. In high-pressure environments such as emergency departments, where time is critical, the ability to obtain immediate results can be the difference between life and death.
- Enhanced Patient Experience
By providing immediate results at the bedside, the HemoScreen eliminates the need for patients to wait for centralized laboratory testing. This reduction in wait time improves the patient experience, particularly in outpatient settings where patients may otherwise face prolonged clinic stays. Additionally, the HemoScreen's ability to perform tests with minimal blood volume (just two drops) reduces the discomfort associated with venipuncture, further enhancing patient satisfaction. This minimally invasive approach is especially beneficial for pediatric patients and those with a fear of needles, making the diagnostic process more comfortable and less stressful.
- Cost-Effectiveness and Resource Optimization
The HemoScreen's point-of-care (POC) capabilities can contribute to cost savings in healthcare systems by reducing the need for centralized laboratory resources and minimizing sample transportation costs. Additionally, its ability to provide rapid results may reduce unnecessary hospitalizations and readmissions, further optimizing resource utilization. The analyzer's low maintenance requirements and disposable cartridge system also contribute to its overall cost-effectiveness. By bringing diagnostic capabilities directly to the patient, the HemoScreen reduces the reliance on centralized laboratories, which can be particularly beneficial in remote or underserved areas where access to laboratory facilities is limited. This not only enhances the efficiency of healthcare delivery but also ensures that patients receive timely and appropriate care, regardless of their location.
Future Directions and Potential Applications
- Expansion into New Clinical Settings
As the HemoScreen continues to gain widespread acceptance across various clinical settings, its potential applications are rapidly expanding. Beyond its current use in primary care, oncology, ICUs, and ORs, the analyzer is poised to find utility in a broader range of healthcare environments. These include pediatric care, where rapid and minimally invasive testing is crucial for young patients; geriatric clinics, where frequent monitoring of blood parameters is essential for managing chronic conditions; and even home healthcare settings, where portability and ease of use make it an attractive option for providing rapid hematology testing. The HemoScreen's compact design and user-friendly interface make it an ideal tool for delivering timely diagnostic information in diverse environments.
- Integration with Digital Health Ecosystems
The integration of the HemoScreen with digital health ecosystems, such as electronic health records (EHRs) and telemedicine platforms, holds significant promise for enhancing healthcare delivery. By enabling seamless data transmission and analysis, this integration can facilitate remote patient monitoring and improve the continuity of care. Clinicians can access real-time hematology results from anywhere, allowing for more informed decision-making and enhanced patient management. This capability is particularly valuable in telemedicine, where remote monitoring can bridge the gap between patients and healthcare providers, ensuring that patients receive timely and appropriate care regardless of their location.
- Ongoing Technological Advancements
As machine vision and AI technologies continue to evolve, the HemoScreen and similar devices will benefit from ongoing improvements in accuracy, speed, and functionality. Future iterations of the HemoScreen may incorporate additional parameters, enhanced diagnostic algorithms, and even predictive analytics capabilities. These advancements will not only improve the precision and efficiency of hematology testing but also enable more sophisticated diagnostic insights. For example, predictive analytics could help identify early signs of disease progression or potential complications, allowing for proactive interventions. By leveraging these technological advancements, the HemoScreen will further solidify its role as a cornerstone of modern healthcare, particularly in the realm of point-of-care hematology testing.
If you have related needs, please feel free to contact us for more information or product support.
Reference
- Bransky, Avishay, et al. "A novel approach to hematology testing at the point of care." The journal of applied laboratory medicine 6.2 (2021): 532-542.
This article is for research use only. Do not use in any diagnostic or therapeutic application.
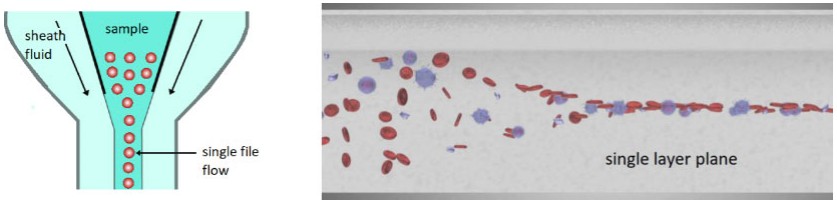 Fig.1 Standard hydrodynamic focusing technique (left) vs viscoelastic focusing (right). (Bransky A., et al., 2021)
Fig.1 Standard hydrodynamic focusing technique (left) vs viscoelastic focusing (right). (Bransky A., et al., 2021)