- Home
- Resource
- Disease Diagnosis
- Infectious Diseases
- Rubella Diagnostics Decoded: From Lab Testing to Congenital Risk Assessment
- Home
- IVD
- By Technology Types
- By Diseases Types
- By Product Types
- Research
- Resource
- Distributors
- Company
Rubella, though preventable, remains a global health threat due to its devastating consequences in pregnancy and challenges in differential diagnosis. This comprehensive resource provides laboratory professionals and public health teams with key insights into rubella detection methods, ranging from established gold-standard techniques (RT-PCR and serology) to emerging innovations. Covering interpretation challenges and specialized applications such as prenatal screening and outbreak response, the resource offers practical guidance to improve test accuracy while supporting global rubella elimination efforts.
Rubella, also known as German measles, is a contagious viral infection caused by the rubella virus, primarily characterized by a mild febrile rash in children and adults. While often benign in healthy individuals, its greatest public health impact lies in congenital rubella syndrome (CRS), a severe condition causing fetal defects (e.g., deafness, cataracts, heart anomalies) when maternal infection occurs during early pregnancy. Due to effective vaccination programs, rubella is now rare in many regions, but outbreaks persist in underimmunized populations, necessitating accurate laboratory diagnosis to distinguish it from other rash illnesses (e.g., measles, parvovirus B19) and guide clinical/public health responses.
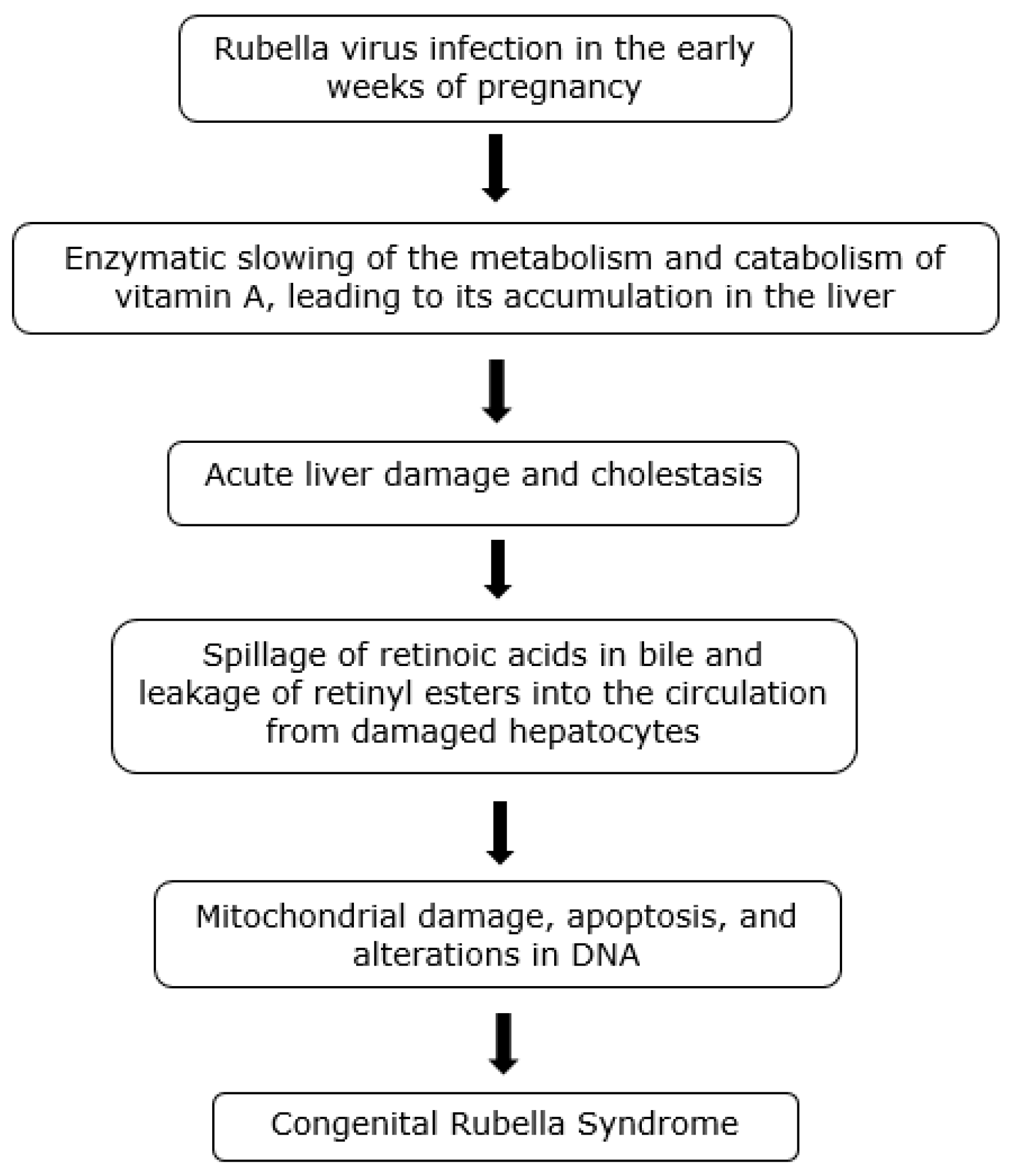 Fig.1 Pathogenesis of the congenital rubella syndrome. (Mawson A R, Croft A M., 2019)
Fig.1 Pathogenesis of the congenital rubella syndrome. (Mawson A R, Croft A M., 2019)
Accurate diagnosis of rubella requires reliable laboratory methods to confirm acute infection, assess immune status, and support public health surveillance. Key techniques include molecular detection for active infection, serological assays for antibody response, and innovative approaches to address emerging challenges in rubella elimination efforts. Below, we explore the three cornerstone methodologies:

RT-PCR
RT-PCR detects rubella virus RNA with high sensitivity, using throat/nasopharyngeal swabs or CSF in congenital cases. It targets conserved regions like the E1 gene, providing results within hours—critical for confirming acute infection and CRS diagnosis. While highly accurate, it requires lab infrastructure and trained staff.
IgM ELISA
IgM ELISA identifies recent rubella infections by detecting virus-specific antibodies in serum, typically appearing 5–14 days post-rash. It’s widely used for prenatal screening and outbreak investigations but may yield false positives in low-prevalence settings due to cross-reactivity.

Emerging Methods
Innovations such as multiplex PCR panels (to detect both rubella and measles), point-of-care tests, and dried blood spot tests (for resource-limited settings) aim to increase the speed, accessibility, and global surveillance of elimination efforts.
Rubella testing requires tailored approaches in high-stakes clinical and public health contexts. Below are key scenarios with interpretation guidelines:

Prenatal rubella screening focuses on assessing maternal immunity (IgG) and detecting acute infection (IgM/IgG avidity) to prevent CRS. For suspected CRS in newborns, RT-PCR testing of urine/oral fluid is preferred over IgM due to higher sensitivity. Timing is critical—low IgG avidity in pregnant women indicates recent infection, requiring close fetal monitoring.

During outbreaks, rapid RT-PCR testing of throat swabs confirms cases within hours, while genotyping distinguishes wild-type from vaccine-derived strains. Public health teams prioritize testing unvaccinated contacts and healthcare workers to contain spread, with results guiding targeted vaccination campaigns.

Post-MMR vaccination, IgM may be transiently positive, complicating acute diagnosis. IgG testing (≥10 IU/mL) confirms immunity, while PCR helps rule out wild-type infection if symptoms appear. Timing matters—testing too early post-vaccine may yield false positives.

Dried blood spot (DBS) testing enables IgG avidity analysis where serum collection is impractical. Syndromic multiplex panels (e.g., rubella/measles/parvovirus) optimize limited resources, though sensitivity may be lower than lab-based PCR. Portable PCR devices are emerging solutions.
Despite significant progress in rubella control, diagnostic challenges persist, particularly in low-prevalence settings, while emerging technologies offer promising solutions for elimination efforts.
Rubella testing faces significant hurdles, including declining clinical suspicion in elimination settings leading to underdiagnosis, high false-positive IgM rates due to cross-reactivity and vaccine interference, and limited access to advanced PCR/genotyping in resource-limited areas. Additionally, diagnosing congenital rubella syndrome (CRS) remains challenging due to the low sensitivity (~50%) of neonatal IgM testing, often requiring confirmatory RT-PCR.
The next generation of rubella diagnostics focuses on multiplex panels (e.g., simultaneous measles/rubella/parvovirus testing), portable molecular tools (microfluidic PCR), and AI-enhanced serology interpretation to reduce false positives. Advances in dried blood spot (DBS) testing and point-of-care IgM/IgG devices aim to expand access in low-resource settings, while global data-sharing platforms could improve outbreak tracking.
Alta DiagnoTech provides comprehensive IVD kits for rubella diagnostics, including RT-PCR assay kits, IgM/IgG ELISA kits, and multiplex panels for precise detection and differentiation. If you have related needs, please feel free to contact us for more information or product support.
Reference
This article is for research use only. Do not use in any diagnostic or therapeutic application.
|
There is no product in your cart. |