- Home
- Resource
- Explore & Learn
- Understanding the Utilization of Clinical Biochemistry Laboratory (CBL) Tests in Hospital Settings
- Home
- IVD
- By Technology Types
- By Diseases Types
- By Product Types
- Research
- Resource
- Distributors
- Company
Clinical Biochemistry Laboratories (CBL) are essential pillars in modern healthcare, providing invaluable diagnostic insights that guide medical decision-making. These laboratories are at the heart of diagnostic and monitoring practices, offering a range of tests that evaluate biochemical markers in body fluids such as blood, urine, and cerebrospinal fluid. The primary role of CBL tests is to assist healthcare professionals in the screening, diagnosis, and management of diseases, making them indispensable in both inpatient and outpatient settings. Despite their critical role, the frequency and patterns of test utilization in clinical biochemistry have received relatively little attention in the medical literature. This article delves into the utilization patterns of CBL tests within hospital environments, providing insights into how often these tests are ordered, which departments rely on them most, and how they contribute to patient care and hospital revenue.
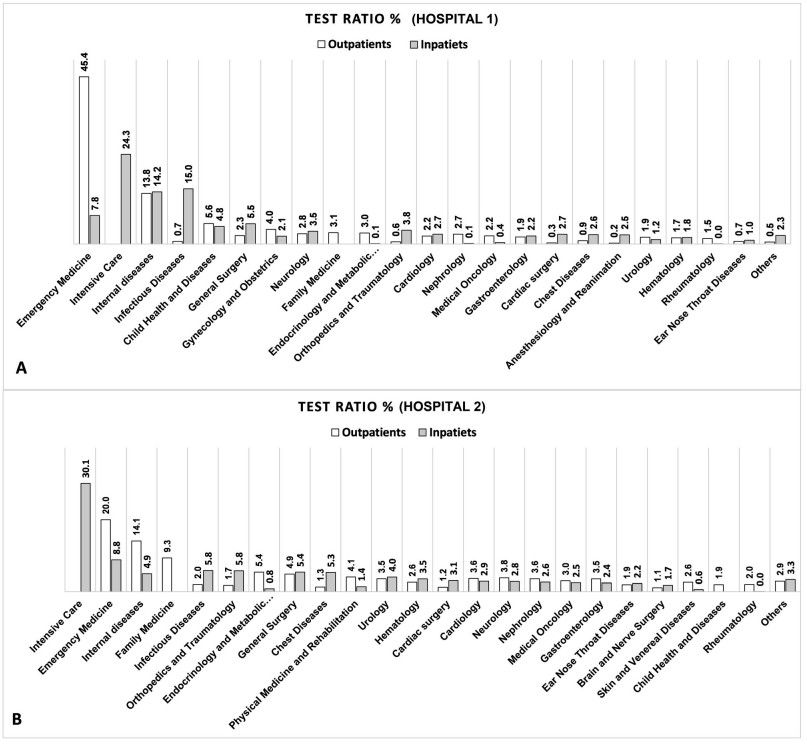 Fig.1 Total test ratio of each department for Hospital 1 (A) and Hospital 2 (B). (Yalçındağ A., et al., 2024)
Fig.1 Total test ratio of each department for Hospital 1 (A) and Hospital 2 (B). (Yalçındağ A., et al., 2024)

CBL tests are indispensable in clinical practice due to their influence on disease detection, prognosis, and treatment. These tests, which include common procedures like Complete Blood Counts (CBC), glucose levels, liver function tests, and kidney function markers, enable doctors to make informed clinical decisions. Studies indicate that laboratory tests influence up to 70% of medical decisions, from initial diagnosis to follow-up care. However, these numbers often go unrecognized by the general public, despite the profound effect laboratory results have on clinical outcomes.
The role of CBL tests is multifaceted: they can help detect diseases early, monitor ongoing treatments, assess organ function, and guide physicians in choosing the appropriate course of action. Moreover, CBLs can help reduce the need for invasive procedures and contribute to preventive healthcare by identifying risk factors before clinical symptoms manifest. These aspects underscore the significance of CBL tests in ensuring that healthcare systems function efficiently and effectively.

This study, conducted across two large hospitals in Turkey between 2018 and 2022, aimed to understand the utilization of CBL tests within hospital settings. The study analyzed over 43 million CBL tests conducted on more than 12 million patients. It focused on understanding which departments used laboratory tests most frequently and explored the variations in test request patterns among different patient groups, particularly outpatients and inpatients.
The hospitals in question were diverse in terms of geography, infrastructure, and patient demographics, offering a comparative view of how CBL tests are utilized in different settings. Despite some differences, the study found that approximately 27-30% of outpatients and 81-89% of inpatients requested at least one CBL test. These figures illustrate the high demand for laboratory testing in both outpatient and inpatient settings, highlighting the central role of CBLs in hospital operations.

Outpatient and Inpatient Trends
The data revealed interesting trends in test utilization across both outpatient and inpatient settings. In Hospital 1, 94% of patients were outpatients, while in Hospital 2, 93% were outpatients. However, despite the high proportion of outpatient visits, a significant number of these patients also required CBL testing. Approximately 27% of outpatients in Hospital 1 and 30.3% in Hospital 2 requested at least one laboratory test during their visit. In contrast, inpatients were far more likely to undergo laboratory testing, with 81.2% to 88.7% of inpatient visits resulting in CBL test orders.
The disparity in test requests between outpatients and inpatients reflects the nature of care provided in hospital settings. Inpatients, particularly those in intensive care units (ICU), tend to require frequent and comprehensive monitoring, which explains the higher number of tests ordered for these patients. The ICU departments in both hospitals had the highest test requests per patient, with an average of 77 to 109 tests ordered for nearly every patient admitted to these units.

Emergency Department Requests
The Emergency Medicine departments were also among the highest users of laboratory tests. In Hospital 1, 19.99% of outpatients requested tests from the Emergency Department, while in Hospital 2, this figure rose significantly to 45.36%. This sharp difference can be attributed to variations in the type of patient population served by each hospital. Emergency departments often deal with acute conditions that require immediate diagnostic information, explaining the higher utilization of laboratory tests in these settings. The demand for CBL testing in emergency departments highlights the need for rapid, accurate diagnostic results to guide the treatment of urgent medical conditions.
The most commonly ordered CBL tests in both hospitals were primarily routine diagnostic tests that assess general health and monitor disease progression. These included:
Additionally, tests like C-reactive protein (CRP) and d-dimer gained prominence in the post-pandemic period, reflecting the global health crisis that elevated the need for inflammatory and coagulation markers to monitor COVID-19 patients.

One of the less frequently discussed aspects of CBL tests is their financial impact on hospital revenue. Despite the relatively low cost of performing many CBL tests, they represent a significant portion of hospital income. In Hospital 1, approximately 50% of laboratory reimbursements were derived from tests such as 25(OH)D, CBC, HbA1c, and d-dimer. Hospital 2 showed similar trends, with tests like d-dimer, troponin, and CRP being significant contributors to laboratory income.
These figures emphasize the dual role of CBL tests: not only do they provide critical diagnostic information, but they also represent a crucial revenue stream for hospitals. The financial contribution of CBL tests, combined with their diagnostic utility, highlights their importance in the broader healthcare ecosystem.
The COVID-19 pandemic had a substantial impact on the patterns of CBL test utilization, particularly for tests related to inflammation, coagulation, and immune response. In Hospital 1, tests for CRP, d-dimer, ferritin, and fibrinogen saw dramatic increases, with some test numbers surging by up to 100 times. This increase in test utilization reflects the heightened need for diagnostic markers to manage and monitor COVID-19 patients, particularly in intensive care settings.
The pandemic also altered the types of tests requested in emergency departments, where the volume of specific tests like d-dimer rose significantly as clinicians sought to understand the thrombotic complications associated with COVID-19. These shifts in test utilization illustrate how global health crises can rapidly change the landscape of laboratory testing, influencing both clinical decisions and hospital operations.
Intensive Care Units (ICUs) are the highest users of laboratory tests in hospitals, as they cater to critically ill patients who require constant monitoring. The data from both hospitals showed that ICU patients typically underwent 77 to 109 tests per patient, with nearly 100% of ICU patients having at least one laboratory test. This high frequency of testing is necessary to track multiple parameters in critically ill patients, including organ function, electrolyte levels, and infection markers.
The extensive use of CBL tests in ICUs is a reflection of the complexity of care required in these units, where doctors need real-time information to make urgent, life-saving decisions. The volume of tests ordered in ICUs underscores the critical role that CBL plays in patient management, especially in high-acuity settings.
The decision to order laboratory tests is not always straightforward, and there are growing concerns regarding the appropriateness of some test requests. Research suggests that up to 20% of test orders may be unnecessary or inappropriate, contributing to unnecessary healthcare costs and potentially putting patients at risk. The phenomenon of Ulysses Syndrome, where unnecessary tests lead to a chain of further procedures and anxiety for patients, is a significant concern in hospital settings.
In many cases, healthcare professionals may order tests excessively due to defensive medicine practices or a lack of clear guidelines on which tests are essential for specific clinical scenarios. Reducing unnecessary test orders is crucial for improving the efficiency of healthcare delivery and minimizing the economic burden on hospital systems.
Clinical Biochemistry Laboratories will continue to play a central role in modern healthcare systems. The data from this study underscores their importance in patient care, particularly in outpatient, emergency, and intensive care settings. The increasing reliance on CBL tests not only reflects their diagnostic value but also their economic impact on hospital revenue generation.
As healthcare systems continue to evolve, there will be a greater emphasis on optimizing the use of laboratory tests to ensure they are ordered appropriately and contribute to improving patient outcomes. Hospitals and clinicians must remain vigilant about test utilization to avoid unnecessary costs and improve the overall efficiency of healthcare systems. Moreover, continued advancements in technology and laboratory medicine will likely further enhance the capabilities of CBLs, ensuring they remain indispensable to patient care and hospital operations.
If you have related needs, please feel free to contact us for more information or product support.
Reference
This article is for research use only. Do not use in any diagnostic or therapeutic application.

Cat.No. GP-DQL-00203
Rotavirus Antigen Group A and Adenovirus Antigen Rapid Test Kit (Colloidal Gold)

Cat.No. GP-DQL-00206
Adenovirus Antigen Rapid Test Kit (Colloidal Gold), Card Style

Cat.No. GP-DQL-00207
Adenovirus Antigen Rapid Test Kit (Colloidal Gold), Strip Style

Cat.No. GP-DQL-00211
Rotavirus Antigen Group A Rapid Test Kit (Colloidal Gold), Card Type

Cat.No. GP-DQL-00212
Rotavirus Antigen Group A Rapid Test Kit (Colloidal Gold), Card Type

Cat.No. IP-00189
Influenza A Rapid Assay Kit

Cat.No. GH-DQL-00200
Follicle-stimulating Hormone Rapid Test Kit (Colloidal Gold)

Cat.No. GH-DQL-00201
Insulin-like Growth Factor Binding Protein 1 Rapid Test Kit (Colloidal Gold)

Cat.No. GH-DQL-00202
Luteinizing Hormone Rapid Test Kit (Colloidal Gold)

Cat.No. GH-DQL-00208
Follicle-stimulating Hormone Rapid Test Kit (Colloidal Gold), Strip Style

Cat.No. GH-DQL-00209
Insulin-like Growth Factor Binding Protein 1 Rapid Test Kit(Colloidal Gold), Strip Style

Cat.No. GH-DQL-00210
Luteinizing Hormone Rapid Test Kit (Colloidal Gold), Strip Style

Cat.No. IH-HYW-0001
hCG Pregnancy Test Strip

Cat.No. IH-HYW-0002
hCG Pregnancy Test Cassette

Cat.No. IH-HYW-0003
hCG Pregnancy Test Midstream

Cat.No. GD-QCY-0001
Cocaine (COC) Rapid Test Kit

Cat.No. GD-QCY-0002
Marijuana (THC) Rapid Test Kit

Cat.No. GD-QCY-0003
Morphine (MOP300) Rapid Test Kit

Cat.No. GD-QCY-0004
Methamphetamine (MET) Rapid Test Kit

Cat.No. GD-QCY-0005
Methylenedioxymethamphetamine ecstasy (MDMA) Rapid Test Kit

Cat.No. GD-QCY-0006
Amphetamine (AMP) Rapid Test Kit

Cat.No. GD-QCY-0007
Barbiturates (BAR) Rapid Test Kit

Cat.No. GD-QCY-0008
Benzodiazepines (BZO) Rapid Test Kit

Cat.No. GD-QCY-0009
Methadone (MTD) Rapid Test Kit

Cat.No. GD-QCY-0011
Opiate (OPI) Rapid Test Kit

Cat.No. ID-HYW-0002
Multi-Drug Test L-Cup, (5-16 Para)

Cat.No. ID-HYW-0005
Multi-Drug Rapid Test (Dipcard & Cup) with Fentanyl

Cat.No. ID-HYW-0006
Multi-Drug Rapid Test (Dipcard & Cup) without Fentanyl

Cat.No. ID-HYW-0007
Multi-Drug 2~14 Drugs Rapid Test (Dipstick & Dipcard & Cup)

Cat.No. ID-HYW-0008
Fentanyl (FYL) Rapid Test (For Prescription Use)

Cat.No. ID-HYW-0009
Fentanyl Urine Test Cassette (CLIA Waived)

Cat.No. ID-HYW-0010
Fentanyl Urine Test Cassette (Home Use)
|
There is no product in your cart. |