The Peripheral Artery Disease (PAD) Diagnostic Pathway: Leveraging Biomarkers for Risk Stratification and Diagnosis
Peripheral artery disease (PAD) is a prevalent circulatory disorder characterized by atherosclerotic narrowing of peripheral arteries, most commonly affecting the lower extremities. This resource details a comprehensive diagnostic approach that integrates functional vascular testing with advanced biomarker analysis to accurately identify PAD and assess its systemic impact. This integrated diagnostic framework enables clinicians to optimize early detection, implement timely interventions, and improve long-term patient outcomes through personalized management strategies.
Introduction to Peripheral Artery Disease (PAD)
Peripheral artery disease (PAD) is a common circulatory disorder characterized by atherosclerotic narrowing of the arteries supplying the limbs, most commonly the lower extremities, leading to reduced blood flow. This condition often manifests as leg pain during walking (claudication) but can progress to rest pain, non-healing wounds, and critical limb ischemia, while also serving as a strong marker for systemic atherosclerosis and elevated cardiovascular risk. Modern diagnosis extends beyond symptomatic assessment to integrate functional vascular testing with biomarker-driven risk stratification, forming a comprehensive approach essential for effective management and prevention of disease progression.
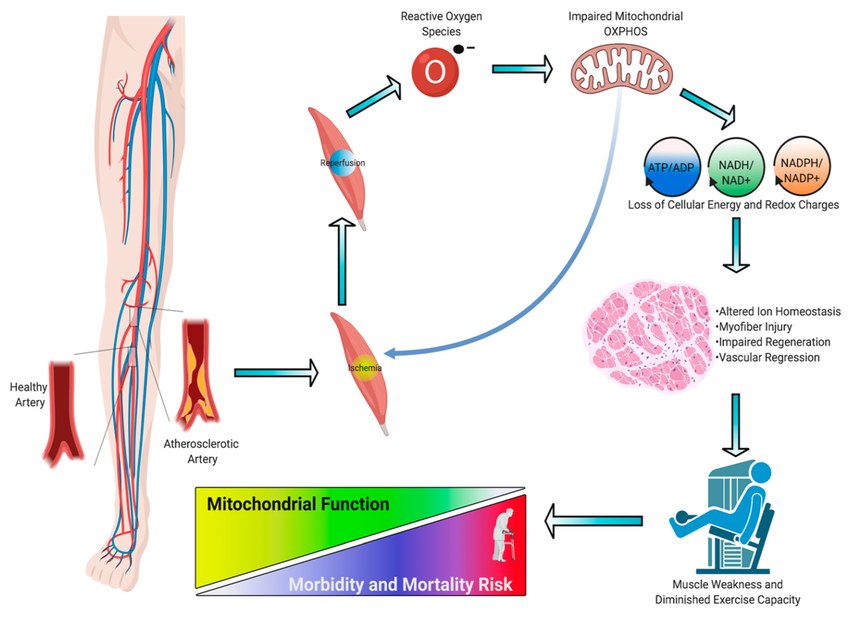 Fig.1 Pathogenesis of ischemic myopathy in peripheral artery disease (PAD). (Kim K, et al., 2020)
Fig.1 Pathogenesis of ischemic myopathy in peripheral artery disease (PAD). (Kim K, et al., 2020)
Clinical Assessment and Functional Testing of Peripheral Artery Disease (PAD)
The diagnosis of peripheral artery disease (PAD) begins with a systematic clinical evaluation followed by objective functional testing to confirm the presence and severity of arterial insufficiency. This foundational stage is crucial for identifying at-risk individuals, differentiating PAD from other conditions with similar symptoms, and establishing a baseline for management. The process integrates targeted physical examination with non-invasive vascular tests that hemodynamically quantify the degree of blood flow impairment.
Clinical Assessment
Clinical assessment starts with a detailed patient history focusing on classic symptoms like claudication (leg pain during walking that resolves with rest), rest pain, and non-healing wounds. The physical exam is pivotal, involving palpation of peripheral pulses (e.g., femoral, popliteal, dorsalis pedis, posterior tibial), auscultation for arterial bruits over major vessels, and inspection of the limbs for skin color changes, temperature, hair loss, and trophic skin changes.
Functional Testing
Functional testing provides objective evidence for diagnosing PAD. The ankle-brachial index (ABI) serves as the cornerstone—a simple, non-invasive test comparing systolic pressure between ankle and arm, with values≤0.90 confirming PAD. For ambiguous cases or non-compressible vessels, the exercise ABI evaluates hemodynamic impact during walking, while the toe-brachial index (TBI) offers a reliable alternative as toe arteries are less affected by calcification. Additionally, doppler and duplex ultrasound visualize blood flow and identify stenosis locations, bridging functional assessment with anatomical imaging.
Key Biomarkers for Peripheral Artery Disease (PAD) Diagnosis
While functional tests confirm impaired blood flow, biomarkers provide critical insights into the underlying causes, systemic impact, and associated risks of peripheral artery disease (PAD). These molecular indicators are essential for comprehensive risk stratification, guiding therapeutic decisions, and managing the overall cardiovascular health of PAD patients.
Lipid Panels & Glucose Metrics
Lipid panels & glucose metrics form the foundation for assessing the atherosclerotic and metabolic risk profile. Measurements of LDL-C and HDL-C directly evaluate the lipid-driven pathophysiology of PAD, while HbA1c and fasting glucose are crucial for diagnosing and monitoring diabetes, a major comorbidity that significantly accelerates disease progression.
Inflammatory Markers
Inflammatory markers reflect the chronic inflammatory component of atherosclerosis. High-sensitivity CRP (hs-CRP) is the most established marker, providing prognostic information on the risk of disease progression and future cardiovascular events beyond traditional risk factors.
Renal Function Markers
Renal function markers are vital as chronic kidney disease is both a risk factor and a consequence of severe PAD. Serum creatinine and cystatin C are used to evaluate glomerular filtration rate, with impaired renal function signaling a more complex clinical course and worse prognosis.
Cardiac-Specific Biomarkers
Cardiac-specific biomarkers address the systemic nature of atherosclerosis by evaluating concomitant heart involvement. BNP/NT-proBNP levels help identify co-existing heart failure, while high-sensitivity cardiac troponin detects subclinical myocardial injury, together refining the overall cardiovascular risk assessment for the patient.
Advanced Imaging for Peripheral Artery Disease (PAD) Diagnosis
Advanced imaging modalities are employed when the diagnosis of PAD requires detailed anatomical mapping for interventional planning or when non-invasive tests yield inconclusive results. These techniques provide high-resolution visualization of the vascular tree, precisely locating stenoses or occlusions, characterizing plaque morphology, and quantifying blood flow. The primary modalities include computed tomography angiography (CTA), which offers rapid, detailed arterial imaging; magnetic resonance angiography (MRA), which avoids ionizing radiation; and the gold standard invasive catheter angiography, which is typically reserved for concurrent therapeutic intervention.
IVD Products for Peripheral Artery Disease (PAD)
Alta DiagnoTech provides a comprehensive suite of in vitro diagnostic (IVD) solutions for peripheral artery disease (PAD), delivering critical biochemical insights that support risk assessment, diagnosis, and management throughout the disease continuum. If you have related needs, please feel free to contact us for more information or product support.
| Product Name |
Technology |
Application |
| Ankle-Brachial Index (ABI) Measurement System |
Doppler Ultrasound/Plethysmography |
Primary non-invasive diagnosis of PAD |
| Lipid Profile Panel |
Enzymatic/Colorimetric Assay |
Assessment of atherosclerotic risk in PAD |
| HbA1c Assay Kit |
High-Performance Liquid Chromatography (HPLC) |
Diabetes screening and monitoring for PAD patients |
| High-Sensitivity CRP (hs-CRP) Test |
Immunoturbidimetric Assay |
Inflammation and cardiovascular risk stratification |
| Cystatin C Assay |
Particle-Enhanced Immunoassay |
Accurate renal function assessment in PAD |
| NT-proBNP Quantitative Assay |
Electrochemiluminescence Immunoassay (ECLIA) |
Heart failure risk evaluation in PAD patients |
| Cardiac Troponin I Assay |
Chemiluminescence Immunoassay (CLIA) |
Detection of myocardial injury in PAD |
Reference
- Kim K, Anderson E M, Scali S T, et al. Skeletal muscle mitochondrial dysfunction and oxidative stress in peripheral arterial disease: a unifying mechanism and therapeutic target[J]. Antioxidants, 2020, 9(12): 1304.
This article is for research use only. Do not use in any diagnostic or therapeutic application.



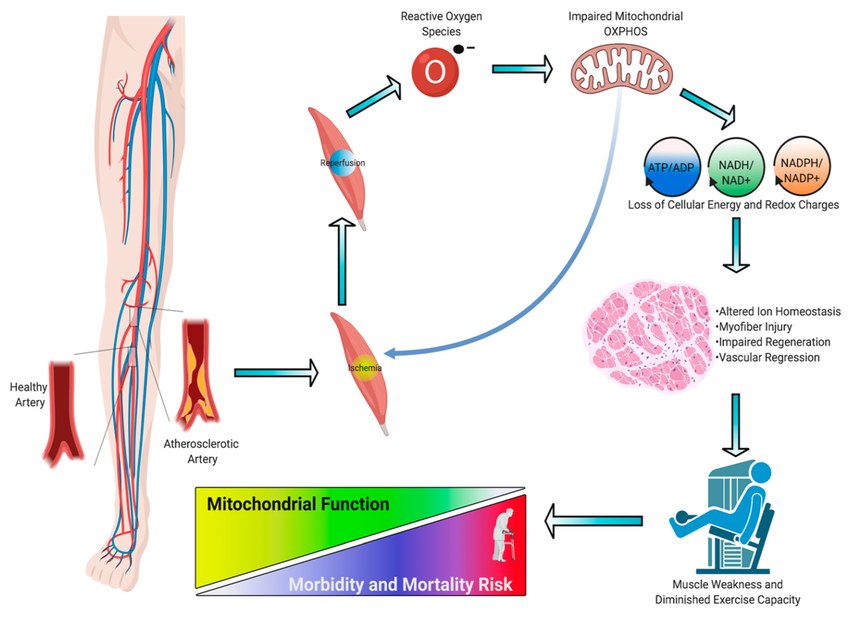 Fig.1 Pathogenesis of ischemic myopathy in peripheral artery disease (PAD). (Kim K, et al., 2020)
Fig.1 Pathogenesis of ischemic myopathy in peripheral artery disease (PAD). (Kim K, et al., 2020) 





