- Home
- Resource
- Disease Diagnosis
- Endocrine Diseases
- The Evolving Landscape of Primary Aldosteronism Diagnosis: From ARR to AVS and Emerging Tools
- Home
- IVD
- By Technology Types
- By Diseases Types
- By Product Types
- Research
- Resource
- Distributors
- Company
Primary aldosteronism (PA) is a common, yet frequently overlooked, endocrine form of hypertension characterized by the autonomous overproduction of aldosterone, leading to significant cardiovascular and renal risks if left undiagnosed. This comprehensive resource page delves into the critical diagnostic pathway for PA, moving from initial clinical suspicion to definitive subtyping. We will explore the essential role of the aldosterone-to-renin ratio (ARR) and its optimization, navigate the confirmatory dynamic functional tests, and examine the pivotal tools for localization—adrenal CT and the gold-standard adrenal vein sampling (AVS).
Primary aldosteronism (PA), once considered a rare cause of hypertension, is now recognized as a common and significant endocrine disorder, accounting for approximately 5-10% of all hypertensive cases. It is characterized by the autonomous overproduction of aldosterone from the adrenal glands, independent of the normal renin-angiotensin system. This excess aldosterone leads to sodium retention, potassium excretion, and increased blood pressure, resulting in a significantly elevated risk of cardiovascular and renal complications—such as stroke, atrial fibrillation, and kidney damage—compared to patients with essential hypertension of similar severity. Timely and accurate diagnosis is therefore critical, as it shifts management from non-specific blood pressure control to targeted therapy, which can include mineralocorticoid receptor antagonist medications or potentially curative adrenalectomy. The diagnostic pathway has evolved into a systematic process involving screening, confirmatory testing, and subtyping, fundamentally aiming to distinguish between unilateral and bilateral disease to guide optimal treatment.
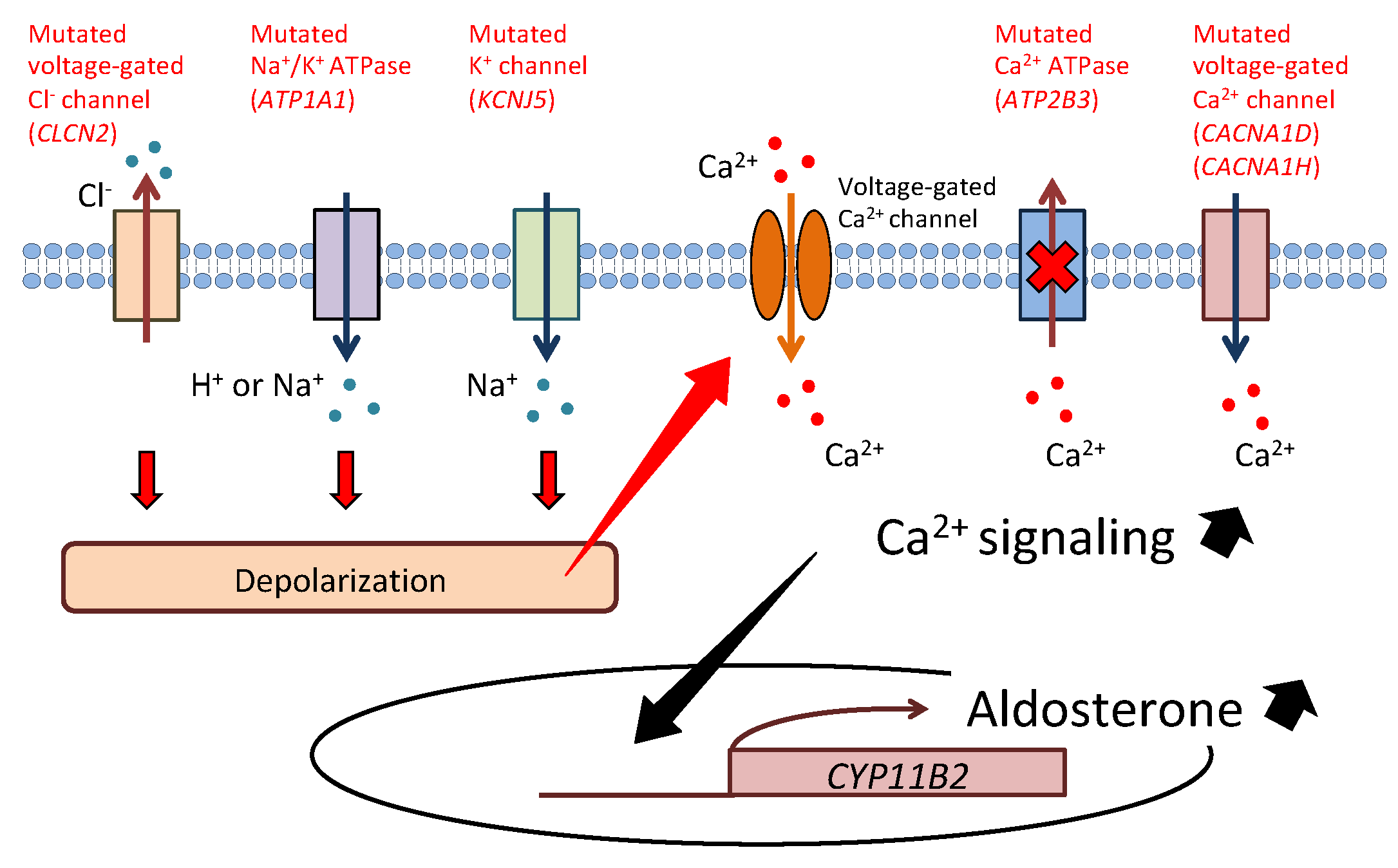 Fig.1 Cellular mechanism of aldosterone synthesis in aldosterone-producing adenoma. (Itcho K, et al., 2021)
Fig.1 Cellular mechanism of aldosterone synthesis in aldosterone-producing adenoma. (Itcho K, et al., 2021)
The aldosterone-to-renin ratio (ARR) serves as the indispensable gateway to diagnosing primary aldosteronism. It is a powerful yet nuanced screening tool designed to detect the characteristic hormonal imbalance of the disease. Its effectiveness, however, hinges entirely on proper execution and interpretation, making an understanding of its core value and optimization critical for any clinician.

The ARR directly reveals the core hormonal characteristic of this disease: abnormally elevated aldosterone levels in the presence of suppressed renin. This simple ratio captures the disrupted physiology of autonomous aldosterone production, enabling the efficient identification of at-risk patients from the broader hypertensive population. Without the ARR as a sensitive and logical first filter, systematic diagnosis and subsequent targeted treatment would not be feasible.

The clinical value of ARR depends entirely on rigorous optimization, as its results are highly susceptible to various variables both before and during analysis. Reliable interpretation requires strict adherence to patient preparation protocols, including medication adjustments, correction of hypokalemia, and control of sodium intake, while also paying close attention to sampling conditions and testing methods. Only through such rigorous methods can ARR serve as a valid and reliable basis for further diagnostic confirmation.
A positive screening test (ARR) alone is not sufficient to diagnose primary aldosteronism (PA), as false positives can occur. The essential next step is confirmatory dynamic functional testing. The core purpose of these tests is to challenge the body's regulatory system and prove that aldosterone production is truly autonomous and nonsuppressible—the defining feature of PA.

Dynamic Functional Testing
The most common tests include the oral sodium loading test, the intravenous saline infusion test (SIT), the captopril challenge test, and the fludrocortisone suppression test. Each test uses a different physiological or pharmacological maneuver (e.g., sodium loading, ACE inhibition) designed to normally suppress aldosterone secretion. In a patient with PA, aldosterone levels remain elevated despite these suppressive challenges.

From Suspected to Confirmed
Crucially, these tests rely on precise and accurate measurement of aldosterone, often at specific time points, to document failed suppression. A positive confirmatory test solidifies the diagnosis of PA and definitively moves the patient from "suspected" to "confirmed," paving the way for the critical final phase: subtyping to determine if the cause is unilateral (surgically curable) or bilateral (managed medically).
Once primary aldosteronism (PA) is biochemically confirmed, the critical next step is subtyping—determining whether the excess aldosterone comes from a single adrenal gland (unilateral disease, often an adenoma) or both glands (bilateral hyperplasia). This distinction is therapeutic, guiding the choice between potential surgical cure (adrenalectomy) and lifelong medical management. The process relies on two complementary yet distinct modalities: anatomical imaging with computed tomography (CT) and functional assessment with adrenal vein sampling (AVS).
Adrenal CT Scan
Adrenal CT scans provide detailed anatomical diagrams and are primarily used to detect large adenomas, assess adrenal cancer, and provide an overall diagnostic roadmap. However, CT scans often miss small aldosterone-secreting adenomas, and frequently identified non-functional nodules can also be misleading. Relying solely on CT for diagnosis can lead to misdiagnosis in nearly 40% of cases.
Adrenal Vein Sampling (AVS)
Adrenal vein sampling (AVS) is therefore considered the diagnostic gold standard for subtyping. It is a technically demanding but essential procedure that directly measures aldosterone and cortisol from each adrenal vein and a peripheral vein. By comparing the hormone gradients, AVS definitively determines if one side is overproducing aldosterone relative to the other (lateralization).
Beyond the established pillars of ARR and AVS, the diagnostic landscape for primary aldosteronism is being reshaped by an emerging toolkit of advanced technologies. These innovations aim to enhance accuracy, simplify the diagnostic pathway, and provide deeper molecular insights, moving towards a more precise and personalized diagnostic paradigm.
Alta DiagnoTech provides a comprehensive in vitro diagnostic (IVD) solution portfolio for primary aldosteronism (PA), supporting the entire diagnostic journey from initial screening to confirmatory testing. Our solutions are built on advanced, precise technologies designed to ensure reliable results at every critical decision point. From automated assays for key biomarkers to sophisticated mass spectrometry for steroid profiling, we empower clinical laboratories to deliver accurate, actionable data, enabling clinicians to effectively diagnose and subtype PA for optimal patient management. If you have related needs, please feel free to contact us for more information or product support.
| Product Name | Technology | Application |
| Aldosterone CLIA Kit | Chemiluminescence Immunoassay (CLIA) | Quantification of serum/plasma aldosterone levels for ARR calculation and dynamic test monitoring. |
| Direct Renin CLIA Kit | Chemiluminescence Immunoassay (CLIA) | Measurement of plasma renin concentration (PRC) for ARR calculation. |
| Steroid Hormone Panel by LC-MS/MS | Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) | Simultaneous, high-specificity quantification of aldosterone, cortisol, 18-oxocortisol, 18-hydroxycortisol for advanced screening, confirmatory testing, and subtyping research. |
Reference
This article is for research use only. Do not use in any diagnostic or therapeutic application.
|
There is no product in your cart. |