Polyarteritis nodosa (PAN) is a rare systemic necrotizing vasculitis targeting medium-sized arteries, whose diagnosis demands a meticulous multimodal approach integrating clinical suspicion, serological exclusion of mimics, and definitive radiographic or histopathological confirmation. This resource delineates the critical role of laboratory testing as the foundational step to rule out alternative vasculitides, while emphasizing the indispensable value of angiography and tissue biopsy for disease verification.
Overview of Polyarteritis Nodosa
Polyarteritis nodosa (PAN) is a rare, systemic necrotizing vasculitis that preferentially targets medium-sized muscular arteries, leading to segmental transmural inflammation, microaneurysm formation, thrombosis, and downstream ischemia or hemorrhage in multiple organs. Classically considered an immune-complex–mediated disease triggered by hepatitis B or, less commonly, other infections, PAN is now classified among the ANCA-negative vasculitides and must be distinguished from overlapping entities such as microscopic polyangiitis and other systemic vasculitides.
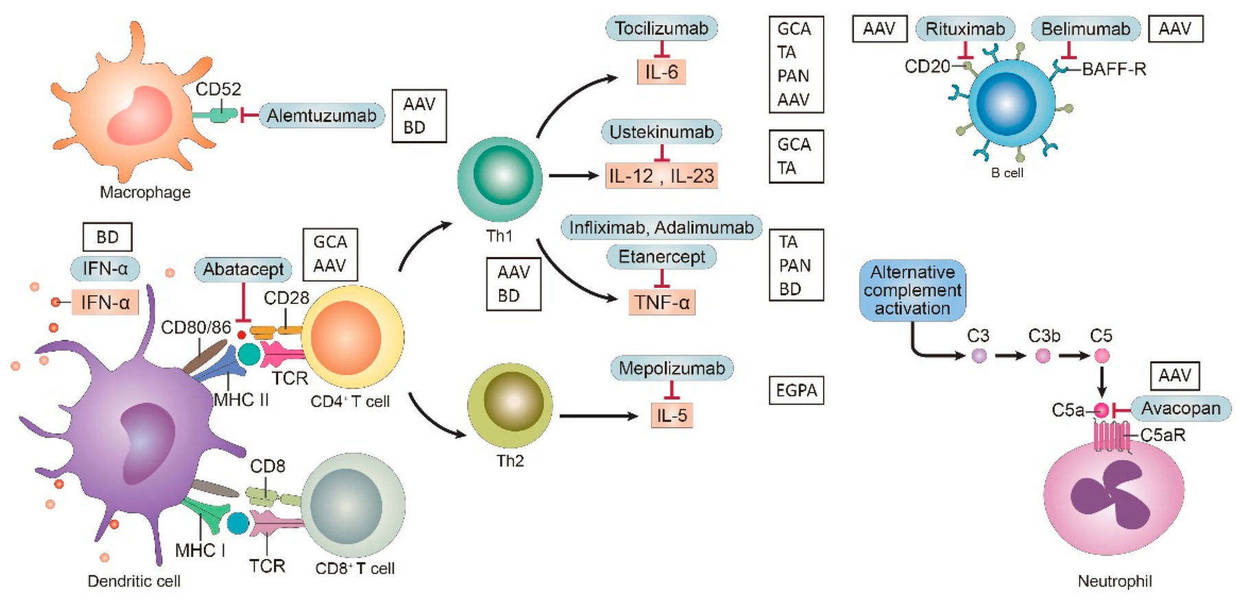 Fig.1 Targets and relative agent in vasculitis. (Chung S W., 2021)
Fig.1 Targets and relative agent in vasculitis. (Chung S W., 2021)
Clinical Suspicion of Polyarteritis Nodosa
Clinical suspicion for polyarteritis nodosa (PAN) arises from the constellation of non-specific systemic symptoms, such as fever, weight loss, and malaise, combined with organ-specific ischemic manifestations resulting from necrotizing inflammation of medium-sized arteries. Key indicators include mononeuritis multiplex (asymmetric peripheral neuropathy), livedo reticularis, testicular pain in males, uncontrolled hypertension, and abdominal pain. This suspicion should prompt immediate serological evaluation to exclude mimics (particularly ANCA-associated vasculitis) and initiate further investigation through angiography or tissue biopsy to confirm the diagnosis.
Serological Exclusion for Polyarteritis Nodosa
Serological testing in polyarteritis nodosa (PAN) operates on a critical paradigm of exclusion rather than confirmation. Unlike many autoimmune diseases where serology identifies pathogenic antibodies, PAN diagnosis primarily relies on ruling out other conditions with similar clinical presentations, particularly ANCA-associated vasculitides (AAV) and hepatitis B virus (HBV)-associated vasculitis. This approach is essential because there is no disease-specific autoantibody for PAN. Instead, serology serves to narrow the differential diagnosis and guide clinicians toward the appropriate confirmatory tests (e.g., angiography or biopsy).
Ruling Out ANCA-Associated Vasculitis (AAV)
ANCA testing is the cornerstone of serological exclusion for PAN, as there is significant clinical overlap between PAN and AAV. A positive ANCA result, particularly for MPO or PR3 antibodies, strongly supports a diagnosis of AAV and effectively rules out classic PAN. ANCA negativity is a prerequisite for considering a definitive PAN diagnosis, ensuring accurate classification and management.
Identifying Hepatitis B Virus (HBV) Association
Testing for HBV infection (HBsAg and anti-HBc) is mandatory in all suspected PAN cases, as HBV can trigger a secondary vasculitis indistinguishable from idiopathic PAN. A positive HBsAg result confirms HBV-associated PAN, fundamentally altering treatment strategies to prioritize antiviral therapy alongside immunosuppression.
Supporting Inflammatory and Hematological Markers
While non-specific, markers like CRP, ESR, and CBC provide objective evidence of systemic inflammation and support the clinical suspicion of active vasculitis. Elevated CRP/ESR, normocytic anemia, leukocytosis, or thrombocytosis reinforce the inflammatory burden but cannot confirm PAN alone. These tests are valuable for monitoring disease activity and treatment response, serving as adjunctive tools within the broader diagnostic framework.
Radiographic and Angiographic Evaluation for Polyarteritis Nodosa
Radiographic and angiographic imaging plays a pivotal role in the diagnosis of Polyarteritis Nodosa (PAN) by providing in vivo visualization of characteristic vascular abnormalities that are often inaccessible to biopsy. While serology excludes mimics and histology offers microscopic confirmation, imaging bridges the gap by non-invasively revealing the extent and distribution of vascular involvement across multiple organ systems.
Conventional Angiography
Conventional catheter-based digital subtraction angiography (DSA) is the historical gold standard for PAN diagnosis due to its superior spatial resolution in visualizing medium-sized arteries. Its pathognomonic findings include microaneurysms (1-5 mm sacculations), segmental stenoses, and the "string of beads" appearance, primarily in renal, hepatic, and mesenteric vessels.
Cross-Sectional Angiography
CT angiography (CTA) and MR angiography (MRA) are non-invasive first-line alternatives for detecting PAN-related vascular lesions. CTA rapidly identifies microaneurysms, stenoses, and organ infarcts with wide availability. MRA avoids radiation and uses less nephrotoxic gadolinium-based contrast, making it safer for serial monitoring, though it has lower spatial resolution.
Other Radiographic Modalities
Doppler ultrasound assesses arterial stenosis and blood flow in accessible vessels but lacks sensitivity for microaneurysms. PET-CT detects generalized vascular inflammation through metabolic activity but is non-specific and cannot differentiate PAN from other vasculitides or infections. These modalities serve adjunctive roles but are not primary tools for PAN confirmation.
Histopathological Confirmation for Polyarteritis Nodosa
Histopathological examination of affected tissue remains the diagnostic gold standard for Polyarteritis Nodosa (PAN), providing definitive evidence of characteristic vascular lesions. The hallmark findings include focal, segmental, transmural necrotizing inflammation of small- to medium-sized arteries, with fibrinoid necrosis, neutrophil infiltration in the acute phase, and mononuclear cells or fibrosis in chronic stages. These changes lead to destruction of the internal elastic lamina and may involve adjacent veins. To maximize diagnostic yield, biopsy should target symptomatic sites (e.g., nerve, muscle, skin, or testicle), as random sampling often fails to capture these patchy lesions. While angiography supports diagnosis, histology offers irreplaceable confirmation and exclusion of other vasculitides.
Alta DiagnoTech offers a comprehensive IVD solution for polyarteritis nodosa, encompassing multiple diagnostic products including ANCA detection kits (MPO/PR3), hepatitis B serology kits (HBsAg/anti-HBc), inflammatory marker test kits (CRP, ESR), and automated platforms supporting key rule-out diagnostics and disease monitoring. If you have related needs, please feel free to contact us for more information or product support.
Reference
- Chung S W. Vasculitis: From target molecules to novel therapeutic approaches[J]. Biomedicines, 2021, 9(7): 757.
This article is for research use only. Do not use in any diagnostic or therapeutic application.



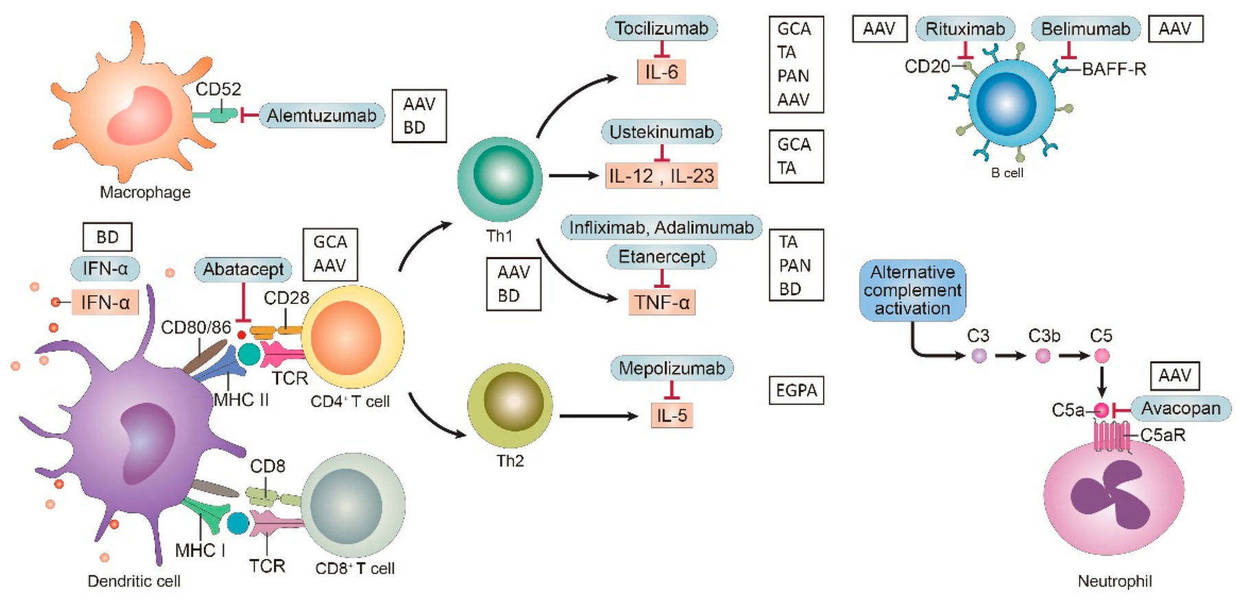 Fig.1 Targets and relative agent in vasculitis. (Chung S W., 2021)
Fig.1 Targets and relative agent in vasculitis. (Chung S W., 2021)