The Diagnostic Blueprint for Primary Hyperparathyroidism: From Abnormal Calcium to Confirmed Diagnosis
Primary hyperparathyroidism (PHPT) is a common endocrine disorder characterized by autonomous overproduction of parathyroid hormone (PTH), leading to hypercalcemia and a spectrum of potential complications. This resource provides a comprehensive, step-by-step blueprint for its diagnosis—from the initial detection of abnormal calcium levels through definitive biochemical confirmation and critical differential diagnosis. We will explore the core biomarkers and essential laboratory workflows that underpin an accurate PHPT diagnosis, concluding with an overview of the specialized in vitro diagnostic (IVD) tools that enable precise and efficient testing.
Introduction to Primary Hyperparathyroidism
Primary hyperparathyroidism (PHPT) is an endocrine disorder characterized by the autonomous overproduction of parathyroid hormone (PTH) from one or more parathyroid glands, leading to disrupted calcium homeostasis. Most often caused by a benign adenoma, PHPT results in hypercalcemia and hypophosphatemia, which can manifest through a wide clinical spectrum—from asymptomatic, incidentally detected biochemical abnormalities to severe complications such as osteoporosis, kidney stones, and neurocognitive symptoms. As the most common cause of outpatient hypercalcemia, its diagnosis hinges on laboratory findings: persistently elevated serum calcium combined with inappropriately normal or elevated PTH levels. Understanding PHPT's pathophysiology and diagnostic pathway is essential for timely intervention and preventing long-term sequelae.
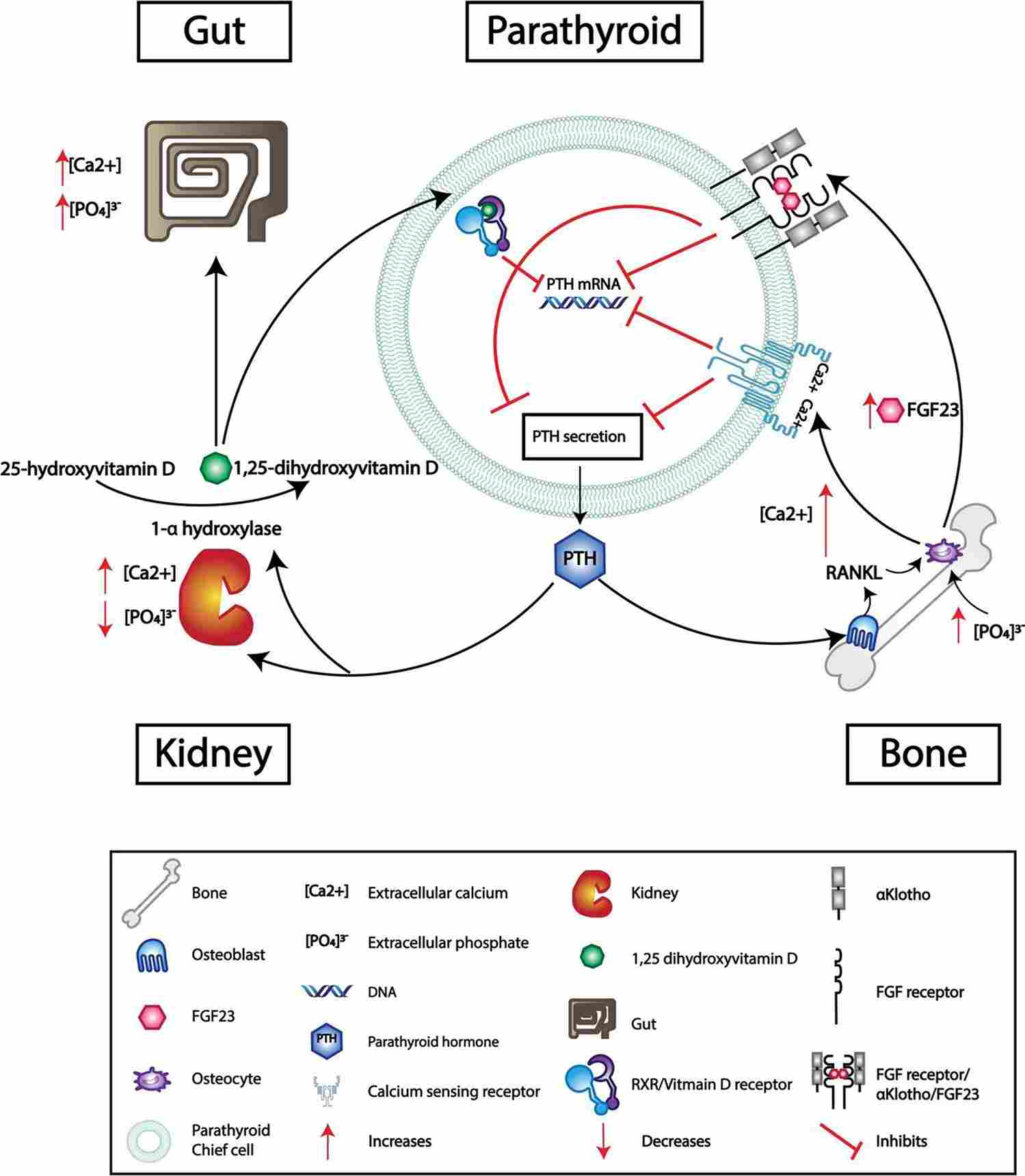 Fig.1 Mechanisms that Inhibit PTH Secretion. (English, Katherine A., et al., 2024)
Fig.1 Mechanisms that Inhibit PTH Secretion. (English, Katherine A., et al., 2024)
Core Biomarkers for Primary Hyperparathyroidism Diagnosis
The biochemical diagnosis of primary hyperparathyroidism (PHPT) is built upon a distinct signature of key biomarkers. The core diagnostic process hinges on demonstrating a simultaneous disruption in serum calcium and parathyroid hormone (PTH) levels, which defines the autonomous and dysregulated state of the parathyroid gland. This signature, supported by discriminatory tests, differentiates PHPT from other causes of hypercalcemia and guides clinical management. The following three aspects form the essential foundation of this diagnostic workup.
Serum Total and Ionized Calcium
Persistent hypercalcemia is the fundamental biochemical trigger for suspecting PHPT. While serum total calcium is the most commonly measured initial test, its interpretation must account for albumin levels, often requiring correction formulas to estimate the physiologically active fraction. For definitive assessment, ionized calcium is the gold standard, as it directly measures the biologically active, unbound calcium in the blood, providing the most accurate reflection of calcium status and confirming true hypercalcemia.
Parathyroid Hormone (PTH)
The measurement of intact PTH is the pivotal and definitive test in the diagnostic cascade. In PHPT, the parathyroid glands secrete PTH autonomously, failing to suppress appropriately in response to elevated calcium levels. Therefore, the hallmark finding is an inappropriately normal or elevated PTH concentration in the setting of confirmed hypercalcemia. Modern, sensitive second-generation PTH immunoassays are critical for accurately capturing this non-suppressed state.
Dysregulation of the PTH-Calcium Axis
The diagnosis of PHPT is confirmed not by isolated values but by demonstrating the broken negative feedback loop between calcium and PTH. In normal physiology, rising calcium levels suppress PTH secretion. In PHPT, this feedback is disrupted. The concurrent presence of hypercalcemia and a non-suppressed PTH level is the pathognomonic biochemical fingerprint of the disease, confirming autonomous parathyroid function and solidifying the diagnosis against other etiologies of hypercalcemia.
Evaluating Incidentally Discovered Hypercalcemia
The evaluation of incidentally discovered hypercalcemia initiates the critical diagnostic pathway for primary hyperparathyroidism (PHPT). This process begins with the essential step of repeating the serum calcium measurement—preferably including ionized calcium—to confirm persistence and exclude transient or factitious causes. Once persistent hypercalcemia is established, the single most important next test is the measurement of intact parathyroid hormone (PTH), as it immediately differentiates between PTH-mediated and non-PTH-mediated etiologies. In this context, a normal or elevated PTH level directly points toward hyperparathyroidism, guiding all subsequent investigations, while a suppressed PTH level shifts the focus to other causes such as malignancy or granulomatous disease. This efficient, two-step biochemical approach ensures a structured and accurate start to the diagnostic workup.
Confirming PHPT and Performing Differential Diagnosis
After confirming persistent hypercalcemia, the diagnostic focus shifts to definitively confirming primary hyperparathyroidism (PHPT) and systematically ruling out other conditions. This phase centers on accurately interpreting the pivotal parathyroid hormone (PTH) result and employing a set of targeted confirmatory and discriminatory laboratory tests. This structured approach is essential to distinguish PHPT from its biochemical mimickers, such as familial hypocalciuric hypercalcemia (FHH) or secondary hyperparathyroidism, ensuring an accurate and actionable diagnosis.
Interpreting the PTH Result
The PTH level, measured in the context of confirmed hypercalcemia, provides the critical directional signal. An elevated or inappropriately normal PTH level strongly indicates a PTH-mediated process, primarily pointing toward PHPT (or, less commonly, tertiary hyperparathyroidism). In contrast, a suppressed or low PTH level effectively rules out PHPT and redirects the investigation toward non-PTH-mediated causes of hypercalcemia, such as malignancy, granulomatous diseases, or medication effects. This single result bifurcates the entire differential diagnostic pathway.
Key Confirmatory & Discriminatory Tests
When PTH is non-suppressed, specific tests are required to confirm PHPT and exclude look-alike conditions. The cornerstone test is the 24-hour urinary calcium excretion (or calcium-creatinine clearance ratio), which is crucial for differentiating PHPT from Familial Hypocalciuric Hypercalcemia (FHH); low urinary calcium supports FHH, while normal or high levels support PHPT. Concurrent measurement of serum phosphate (often low in PHPT due to renal wasting) and 25-hydroxyvitamin D (to exclude deficiency-driven secondary hyperparathyroidism) completes the essential biochemical profile for a definitive diagnosis.
IVD Products for Primary Hyperparathyroidism
Alta DiagnoTech offers a comprehensive portfolio of in vitro diagnostic (IVD) solutions to support the accurate and efficient diagnosis of primary hyperparathyroidism (PHPT). Our integrated systems cover the entire diagnostic pathway—from initial calcium screening to definitive PTH measurement and critical confirmatory tests—enabling laboratories to deliver precise, timely results that guide clinical decision-making. If you have related needs, please feel free to contact us for more information or product support.
| Product Name |
Technology |
Application |
| Intact PTH Immunoassay |
Chemiluminescent Immunoassay (CLIA) |
Quantitative measurement of intact parathyroid hormone in serum/plasma. |
| Total Calcium Detection Reagent |
Colorimetric / Arsenazo III Method |
Accurate determination of total serum calcium levels. |
| Ionized Calcium Analyzer |
Ion-Selective Electrode (ISE) |
Direct measurement of biologically active ionized calcium in whole blood. |
| 25-Hydroxyvitamin D Assay |
Enzyme-Lmunoassay (EIA) / CLIA |
Assessment of vitamin D status to rule out secondary hyperparathyroidism. |
| Urinary Calcium Detection Kit |
Colorimetric / Cresolphthalein Complexone Method |
Quantification of calcium in 24-hour urine collections. |
| Phosphorus (Inorganic) Assay |
UV-Enzymatic / Phosphomolybdate Method |
Measurement of serum phosphate levels to assess renal phosphate wasting. |
| Automated Bone Turnover Panel |
CLIA / EIA |
Simultaneous detection of CTX and bone-specific alkaline phosphatase (BALP). |
| Albumin Detection Reagent |
Bromocresol Green (BCG) Method |
Serum albumin measurement for corrected calcium calculation. |
Reference
- English, Katherine A., Kate E. Lines, and Rajesh V. Thakker. "Genetics of hereditary forms of primary hyperparathyroidism." Hormones 23.1 (2024): 3-14.
This article is for research use only. Do not use in any diagnostic or therapeutic application.



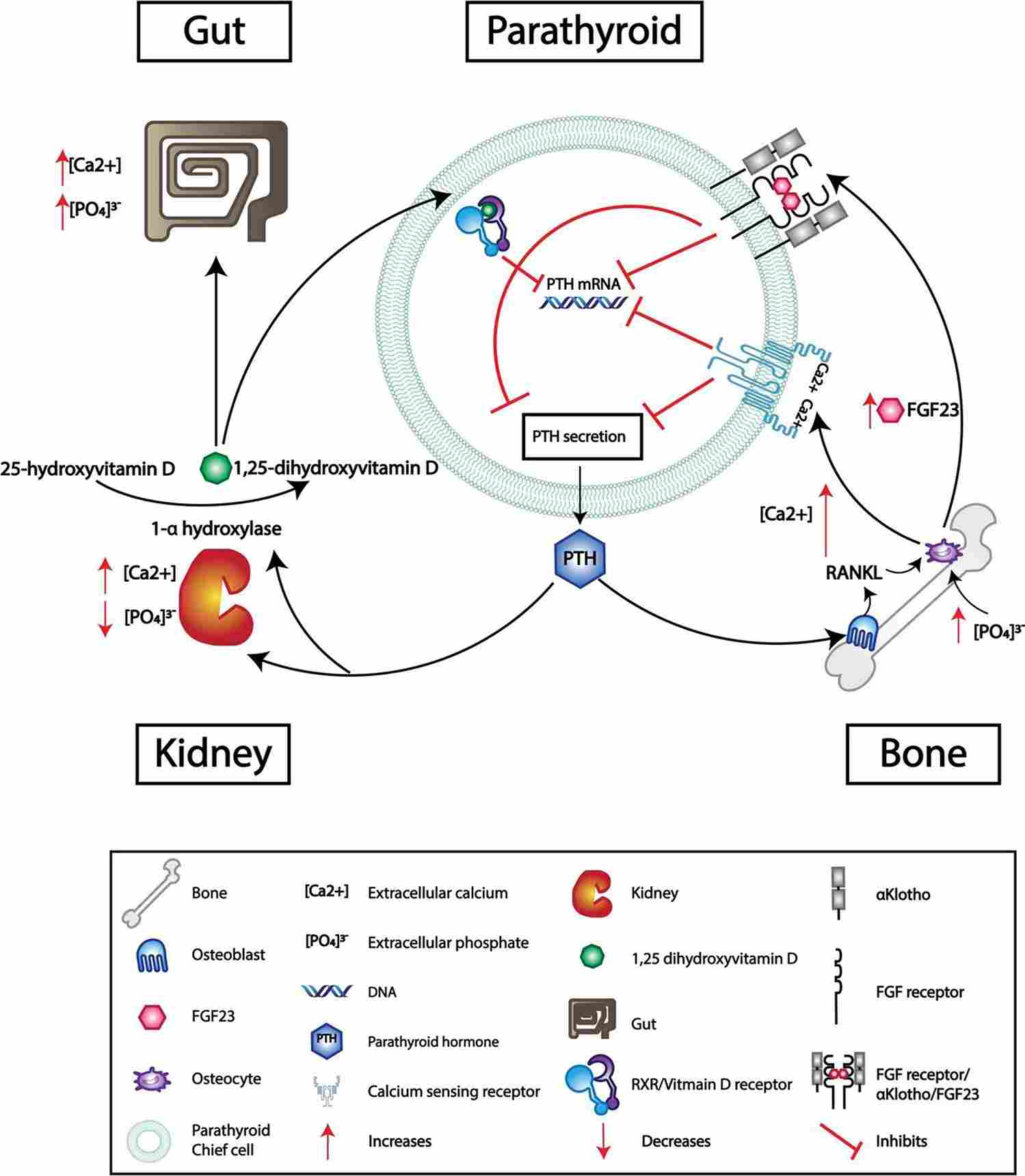 Fig.1 Mechanisms that Inhibit PTH Secretion. (English, Katherine A., et al., 2024)
Fig.1 Mechanisms that Inhibit PTH Secretion. (English, Katherine A., et al., 2024)