- Home
- Resource
- Disease Diagnosis
- Endocrine Diseases
- The Cushing's Syndrome Testing Cascade: A Stepwise Biochemical Strategy
- Home
- IVD
- By Technology Types
- By Diseases Types
- By Product Types
- Research
- Resource
- Distributors
- Company
Cushing's syndrome is an endocrine disorder characterized by chronic exposure to excess cortisol, leading to a complex array of metabolic and physical manifestations. This resource provides a comprehensive guide to the systematic diagnostic cascade for Cushing's syndrome, detailing the essential biochemical tests and stepwise strategy for confirming hypercortisolism, determining its ACTH dependency, and differentiating between pituitary and ectopic sources to guide targeted treatment decisions.
Cushing's syndrome is an endocrine disorder characterized by chronic exposure to excessively high levels of cortisol, the body's primary stress hormone. This condition can result from either endogenous overproduction, often due to pituitary or adrenal tumors, or prolonged exogenous administration of glucocorticoid medications. The syndrome manifests through distinctive clinical features including central obesity, moon face, purple striae, hypertension, and glucose intolerance, though presentation can be highly variable. Diagnosis requires a systematic biochemical approach to confirm inappropriate cortisol secretion and determine the underlying etiology, as accurate differentiation between pituitary, adrenal, and ectopic sources is crucial for determining appropriate treatment strategies ranging from surgical intervention to medical management.
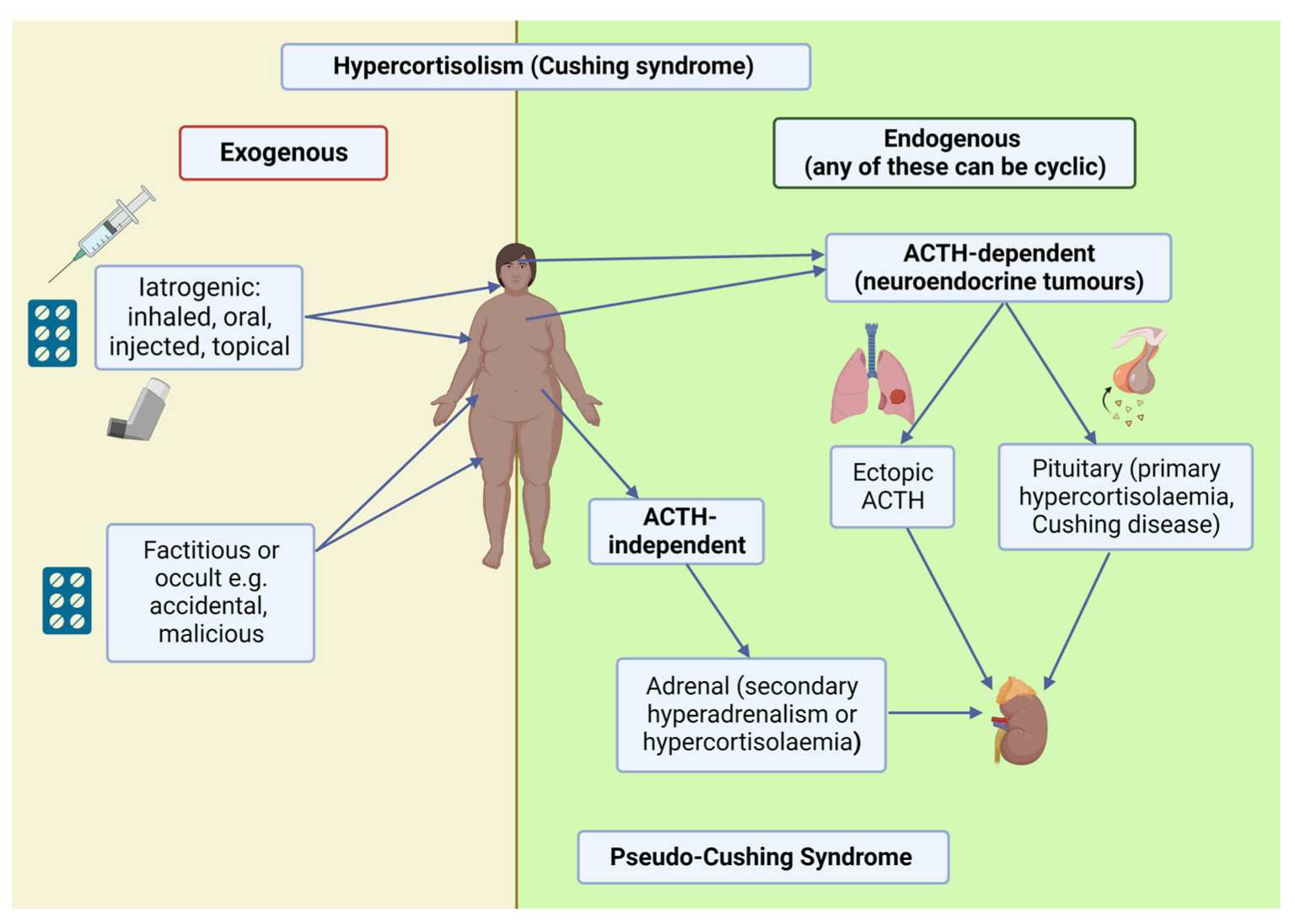 Fig.1 Causes and nomenclature of hypercortisolism (Cushing syndrome) in humans. (Flowers K C, Shipman K E., 2023)
Fig.1 Causes and nomenclature of hypercortisolism (Cushing syndrome) in humans. (Flowers K C, Shipman K E., 2023)
The initial and most critical step in diagnosing Cushing's syndrome is to biochemically confirm the presence of pathological cortisol excess. This phase focuses on distinguishing true endogenous hypercortisolism from pseudo-Cushing states (such as those caused by obesity, chronic stress, or alcoholism) through a series of carefully selected tests. The goal is to demonstrate the loss of normal cortisol regulation by showing elevated cortisol production and disrupted circadian rhythm. Key diagnostic approaches include:

24-Hour Urinary Free Cortisol (UFC) Measurement
This test provides an integrated assessment of cortisol production over a full day and is considered one of the most reliable screening methods. Elevated levels on two or more collections strongly suggest Cushing's syndrome.
Late-Night Salivary Cortisol Testing
This convenient and sensitive method detects the loss of diurnal cortisol rhythm, a hallmark of Cushing's syndrome. Elevated levels between 11 PM and midnight are highly suggestive of the condition.

Dexamethasone Suppression Tests
The overnight dexamethasone suppression test is a widely used screening tool where failure to suppress cortisol levels after taking 1 mg of dexamethasone indicates autonomous cortisol production. The low-dose dexamethasone suppression test (0.5 mg every 6 hours for 48 hours) provides more definitive evidence of pathological cortisol excess.

Interpretation Considerations
At least two different abnormal tests are typically required to confirm the diagnosis, as no single test is perfect. Factors such as medications, concurrent illnesses, and proper test execution can significantly impact results and must be considered in interpretation.
Once Cushing's syndrome is confirmed, determining its underlying cause is essential for guiding appropriate treatment, and ACTH testing serves as the critical first step in this etiological investigation. Measuring plasma ACTH levels effectively distinguishes between ACTH-dependent and ACTH-independent causes, creating a fundamental branching point in the diagnostic pathway and directing all subsequent evaluation. Key aspects of ACTH testing include:

Detectable or elevated ACTH levels indicate that the source of excess cortisol is outside the adrenal glands, driven by either a pituitary adenoma (Cushing's disease) or an ectopic ACTH-secreting tumor. This result necessitates further testing, such as the high-dose dexamethasone suppression test or inferior petrosal sinus sampling, to differentiate between these two possibilities.

Suppressed or undetectable ACTH levels point to a primary adrenal cause, such as an adrenal adenoma, carcinoma, or hyperplasia. In this scenario, the adrenal gland produces cortisol autonomously, and the normal pituitary ACTH production is suppressed via negative feedback. This finding directs the focus toward adrenal imaging.

Accurate measurement requires a reliable ACTH assay, and proper sample handling is crucial due to the hormone's instability. The test should be performed when hypercortisolism is biochemically active, and results must be interpreted in the context of the overall clinical picture, as some ectopic tumors can produce variable ACTH levels.

After confirming ACTH-dependent Cushing's syndrome through elevated or inappropriately normal ACTH levels, the critical next step is to distinguish between its two primary causes: Cushing's disease (a pituitary adenoma) and ectopic ACTH syndrome (a non-pituitary tumor). This differentiation is crucial as it determines the treatment pathway—transsphenoidal surgery for pituitary sources versus localization and resection of an ectopic tumor. The process relies on dynamic endocrine testing that exploits the physiological differences between these etiologies, primarily assessing the tumor's response to glucocorticoid negative feedback and CRH stimulation.
Navigating the complex diagnostic journey of Cushing's syndrome requires precise biochemical evidence. Alta DiagnoTech delivers this critical capability through a specialized portfolio of advanced in vitro diagnostic (IVD) solutions that empower clinicians to reliably confirm hypercortisolism, pinpoint its underlying cause, and make informed treatment decisions based on accurate hormone measurement data. If you have related needs, please feel free to contact us for more information or product support.
| Product Name | Technology | Application |
| Salivary Cortisol Detection Kit | Chemiluminescent Immunoassay (CLIA) | Non-invasive assessment of late-night cortisol levels for initial screening of Cushing's syndrome |
| 24-Hour Urinary Free Cortisol Assay | Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) | Gold-standard quantification of total cortisol production over 24 hours |
| Plasma ACTH Detection Kit | Chemiluminescent Immunoassay (CLIA) | Differential diagnosis of ACTH-dependent vs. ACTH-independent Cushing's syndrome |
| Dexamethasone Suppression Test Panel | Automated Immunoassay System | Comprehensive evaluation of cortisol suppression capacity for diagnostic confirmation |
| CRH Stimulation Test Assay Panel | Chemiluminescent Immunoassay (CLIA) | Differentiation between pituitary and ectopic sources of ACTH in ACTH-dependent Cushing's syndrome |
Reference
This article is for research use only. Do not use in any diagnostic or therapeutic application.
|
There is no product in your cart. |