Celiac disease is an autoimmune disorder triggered by gluten that requires a specific two-step process for accurate diagnosis. This resource details the established celiac disease diagnostic pathway, providing a clear guide from initial clinical suspicion and serologic testing using key biomarkers like tTG-IgA, through to definitive histological confirmation via duodenal biopsy, and explains how these components are integrated into a stepwise diagnostic algorithm.
Overview of Celiac Disease
Celiac disease is a chronic autoimmune disorder in which the ingestion of gluten (a protein found in wheat, barley, and rye) triggers an immune response that attacks the lining of the small intestine. This damage, characterized by villous atrophy, impairs nutrient absorption and can lead to a wide range of gastrointestinal and systemic symptoms, including diarrhea, abdominal pain, fatigue, anemia, and dermatitis herpetiformis. Diagnosis is confirmed through a two-step process: initial screening with specific serologic blood tests (primarily for IgA tissue transglutaminase antibodies) followed by a definitive duodenal biopsy obtained via endoscopy to visualize the characteristic intestinal damage, all while the patient is on a gluten-containing diet.
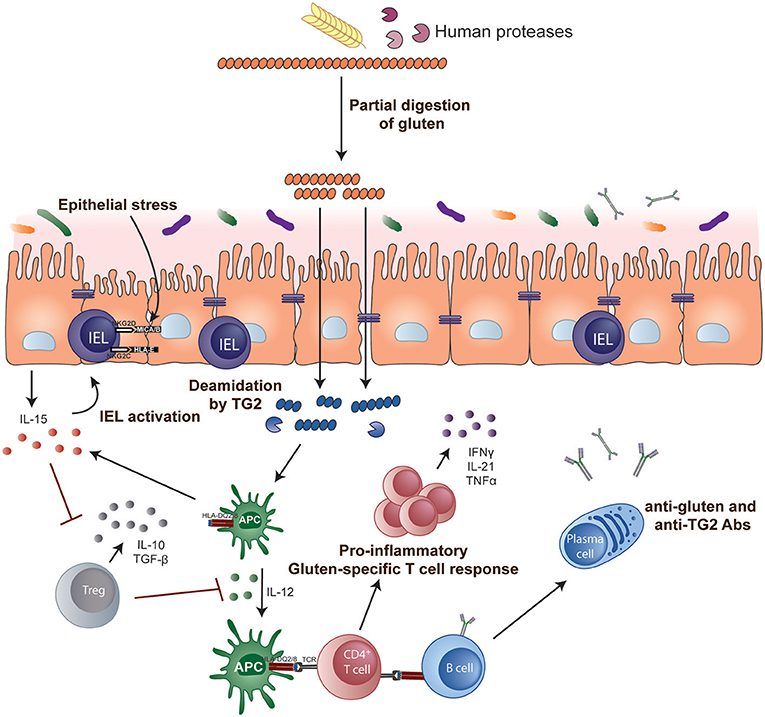 Fig.1 Key steps in celiac disease pathogenesis. (Tye-Din, Jason A., et al., 2018)
Fig.1 Key steps in celiac disease pathogenesis. (Tye-Din, Jason A., et al., 2018)
Clinical Suspicion and Pre-Testing Preparation
Clinical suspicion for celiac disease should arise from a combination of symptomatic presentations, which can be classic (chronic diarrhea, weight loss, bloating) or non-classical/extraintestinal (iron-deficiency anemia, fatigue, dermatitis herpetiformis, elevated liver enzymes), and the presence of associated conditions such as type 1 diabetes or autoimmune thyroid disease. The single most critical step in pre-testing preparation is ensuring the patient is on a gluten-containing diet at the time of testing; initiating a gluten-free diet before diagnostic evaluation can lead to false-negative serology and biopsy results, effectively masking the disease and preventing an accurate diagnosis.
Serologic Testing of Celiac Disease
Serologic testing is the critical first-line laboratory tool for screening individuals with suspected celiac disease. It detects specific antibodies produced by the immune system in response to gluten, providing a sensitive and non-invasive indicator that guides the decision to proceed with definitive biopsy confirmation.
Primary Biomarkers
The primary biomarkers for serologic testing are IgA-class autoantibodies. The IgA tissue transglutaminase (tTG-IgA) antibody test is recommended as the single best first-line screening test due to its high sensitivity and specificity. The IgA endomysial antibody (EMA) test is highly specific and is often used as a confirmatory test following a positive tTG-IgA result, though its interpretation can be more subjective.
Important Considerations
A crucial pre-analytical consideration is the patient's diet, as tests are only accurate if the individual is on a gluten-containing diet. A key laboratory consideration is assessing total serum IgA levels to rule out selective IgA deficiency, which is more common in celiac patients and can lead to false-negative results on standard IgA-based tests; in such cases, IgG-based antibody tests (e.g., tTG-IgG, DGP-IgG) must be used.
Duodenal Biopsy for Celiac Disease Diagnosis
Duodenal biopsy, obtained via upper endoscopy, represents the definitive gold standard for confirming the diagnosis of celiac disease. It provides direct visual and microscopic evidence of the small intestinal damage caused by the autoimmune response to gluten, which is required to finalize the diagnosis following positive serologic testing.
Histological Assessment
Histological assessment of the biopsy samples involves examining the tissue architecture under a microscope, typically using the Marsh-Oberhuber classification. This system grades the severity of characteristic changes: increased intraepithelial lymphocytes (IELs), crypt hyperplasia (elongation), and most importantly, the degree of villous atrophy, ranging from partial blunting to total flattening of the absorptive villi.
Key Principle
The key principle in diagnosis is that a positive duodenal biopsy showing compatible damage (typically Marsh type 2 or 3) is mandatory to confirm celiac disease in adults, even in the presence of positive serology. The biopsy does not stand alone; it integrates with serologic findings to provide the conclusive evidence of the disease process, ensuring diagnostic accuracy and ruling out other causes of enteropathy.
Diagnostic Algorithm of Celiac Disease
The diagnostic algorithm for celiac disease is a standardized, stepwise pathway designed to objectively confirm the condition. It systematically integrates clinical evaluation, specific serologic testing, and definitive histologic examination, with the critical requirement that the patient consumes gluten throughout the process to ensure test accuracy.
- Step 1: Clinical Evaluation and Dietary Preparation: The process begins with assessing symptoms or risk factors that warrant testing, and crucially, ensuring the patient is on a gluten-containing diet to avoid false-negative results.
- Step 2: First-Line Serologic Screening: The initial laboratory test is the IgA tissue transglutaminase (tTG-IgA) antibody blood test, which has high sensitivity and specificity for screening; a concurrent total serum IgA level is checked to rule out IgA deficiency.
- Step 3: Serologic Interpretation and Next Steps: If the tTG-IgA test is positive and the patient has normal total IgA, the next step is referral for a duodenal biopsy; if the test is negative but clinical suspicion remains high, IgG-based tests or HLA genotyping may be considered.
- Step 4: Definitive Histologic Confirmation: A diagnosis is confirmed only if the duodenal biopsy, obtained via endoscopy, shows the characteristic microscopic damage (villous atrophy) consistent with celiac disease, according to standardized classification systems (e.g., Marsh-Oberhuber).
- Step 5: Integration and Final Diagnosis: A final diagnosis of celiac disease is established only when both the positive serology (Step 2) and compatible histology (Step 4) are present, fulfilling the essential diagnostic criteria.
IVD Products for Celiac Disease
To support the precise and standardized diagnostic pathway for celiac disease, Alta DiagnoTech provides a comprehensive portfolio of in vitro diagnostic (IVD) solutions. Our assays and systems are designed to facilitate every critical step, from initial serologic screening and rule-out testing to providing insights for clinical decision-making, ensuring laboratories can deliver accurate results for definitive diagnosis. If you have related needs, please feel free to contact us for more information or product support.
| Product Name |
Technology |
Application |
| Tissue Transglutaminase IgA (tTG-IgA) Antibody Assay Kit |
Chemiluminescent Immunoassay (CLIA) |
Quantitative measurement of tTG-IgA antibodies for first-line serologic screening of celiac disease. |
| Total IgA Quantification Assay Kit |
Immunoturbidimetry |
Measurement of total serum IgA to rule out IgA deficiency and ensure accurate interpretation of IgA-based celiac serology. |
| Deamidated Gliadin Peptide (DGP) IgG/IgA Antibody Assay Kit |
Enzyme-Linked Immunosorbent Assay (ELISA) |
Detection of DGP antibodies as an alternative serologic test, particularly in cases of selective IgA deficiency. |
| Celiac Disease HLA-DQ2/DQ8 Genotyping Kit |
Real-Time PCR |
Detection of HLA-DQ2 and HLA-DQ8 alleles to assess genetic risk; a negative result has high negative predictive value for ruling out celiac disease. |
| Endomysial Antibody (EMA) IgA Testing Kit |
Indirect Immunofluorescence (IIF) |
Qualitative detection of EMA-IgA antibodies, used as a highly specific confirmatory test following a positive tTG-IgA result. |
| Automated Celiac Disease Serology Testing System |
Automated Immunoassay Platform |
A high-throughput, automated system for running tTG-IgA and other related assays, improving laboratory workflow efficiency and standardization. |
Reference
- Tye-Din, Jason A., Heather J. Galipeau, and Daniel Agardh. "Celiac disease: a review of current concepts in pathogenesis, prevention, and novel therapies." Frontiers in pediatrics 6 (2018): 350.
This article is for research use only. Do not use in any diagnostic or therapeutic application.



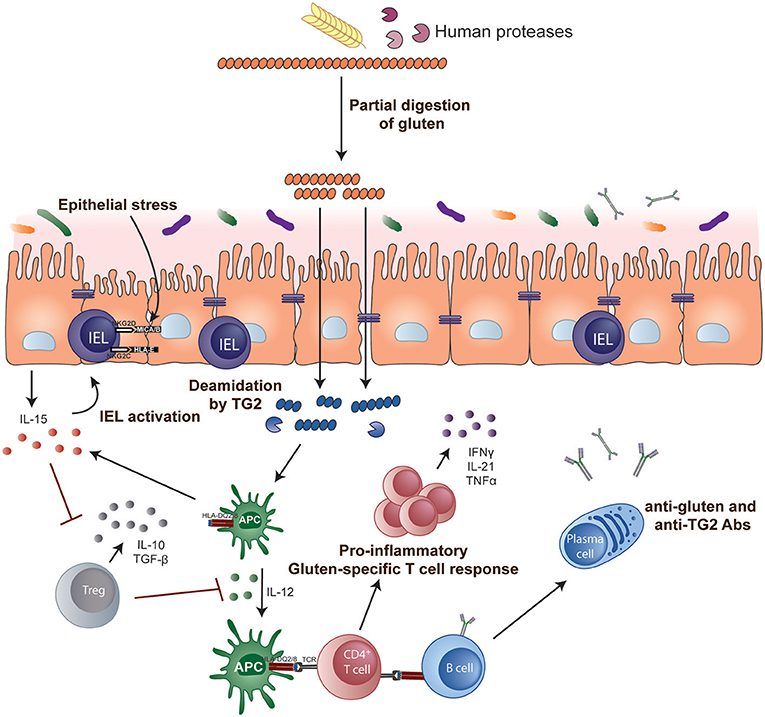 Fig.1 Key steps in celiac disease pathogenesis. (Tye-Din, Jason A., et al., 2018)
Fig.1 Key steps in celiac disease pathogenesis. (Tye-Din, Jason A., et al., 2018)