- Home
- Resource
- Disease Diagnosis
- Infectious Diseases
- Standardizing Tetanus Diagnosis: From Clinical Suspicion to Lab-Assisted Management
- Home
- IVD
- By Technology Types
- By Diseases Types
- By Product Types
- Research
- Resource
- Distributors
- Company
Tetanus is a life-threatening but preventable disease that is challenging to diagnose due to its reliance on clinical evaluation and the lack of definitive laboratory tests. This resource provides healthcare professionals with a comprehensive modern reference for tetanus diagnosis, encompassing clinical suspicion, traditional laboratory diagnosis, laboratory-assisted strategies (such as antitoxin titer kits and wound PCR for borderline cases), and emerging technologies that may revolutionize testing.
Tetanus is a life-threatening neurological disease caused by Clostridium tetani toxin, typically entering through contaminated wounds. Despite being vaccine-preventable, it remains a global health concern due to incomplete immunization and diagnostic challenges. The disease manifests with severe muscle spasms, rigidity, and autonomic dysfunction, requiring immediate clinical suspicion and treatment. Current diagnostics rely primarily on symptom recognition, as traditional methods (culture, PCR) lack sensitivity. This underscores the critical need for standardized clinical pathways and adjuvant laboratory tools to support rapid decision-making in suspected cases.
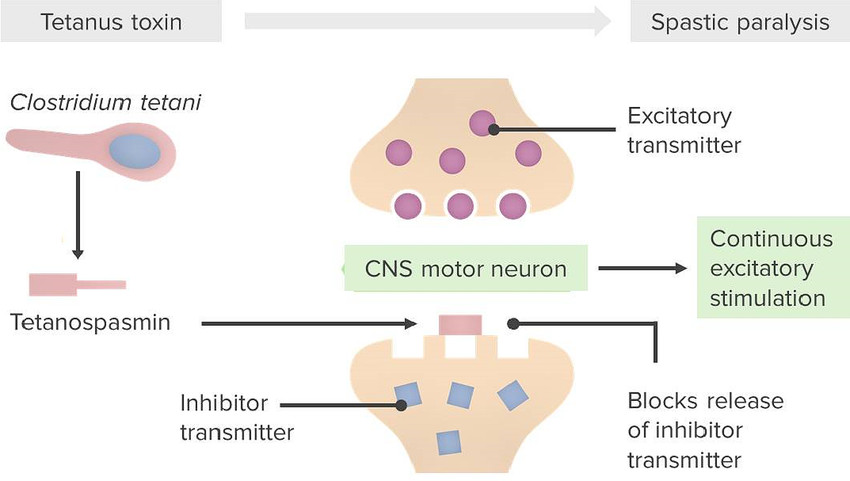 Fig.1 Illustration of the mechanism of action of tetanus toxin. (Boer, Menno, et al., 2024)
Fig.1 Illustration of the mechanism of action of tetanus toxin. (Boer, Menno, et al., 2024)
Tetanus is primarily a clinical diagnosis, as laboratory tests often lack sensitivity and timeliness. Prompt recognition of symptoms is critical due to the disease's rapid progression and high mortality.
Tetanus is diagnosed clinically through hallmark signs: trismus (”lockjaw”), risus sardonicus (characteristic grimace), and generalized muscle spasms triggered by stimuli. Autonomic dysfunction (e.g., labile blood pressure) and a history of wound exposure further support the diagnosis. Unlike other infections, tetanus typically presents without fever, helping distinguish it from sepsis or CNS infections.
Critical mimics include strychnine poisoning (similar spasms but no trismus), drug-induced dystonia (e.g., metoclopramide), and hypocalcemia (positive Chvostek's/Trousseau's signs). Meningitis/encephalitis can be excluded by normal CSF analysis and the absence of trismus. Rapid clinical differentiation is vital to avoid delayed treatment.
| Grade | Severity | Key Clinical Features |
| Grade I | Mild | Localized muscle rigidity/spasms, mild trismus, no respiratory involvement |
| Grade II | Moderate | Moderate trismus/dysphagia, generalized spasms (no apnea), mild autonomic symptoms |
| Grade III | Severe | Severe generalized spasms, respiratory compromise (apnea risk), tachycardia/hypertension |
| Grade IV | Very Severe | Life-threatening spasms, severe autonomic dysfunction (labile BP, arrhythmias), high mortality risk |
Tetanus remains primarily a clinical diagnosis, but laboratory methods can play a supportive role in atypical cases or epidemiological investigations. However, current techniques face significant limitations in sensitivity and practicality, often rendering them unreliable for acute clinical decision-making. Below, we outline the available diagnostic approaches and their key constraints.

Wound culture and PCR for Clostridium tetani are occasionally attempted but suffer from low sensitivity (<30%). Serological tests measuring antitoxin antibody titers (via ELISA) may help assess vaccination status but cannot confirm active infection. Research-stage toxin detection assays (e.g., for tetanospasmin) show promise but remain experimental. These tools are most useful for epidemiological surveillance or excluding differential diagnoses rather than acute case confirmation.

The fastidious nature of C. tetani and low bacterial loads render culture and PCR frequently negative, even in confirmed cases. Antibody titer interpretation is complicated by prior vaccination or immunoglobulin administration. No existing test meets gold standard criteria, and results often come too late to guide initial treatment decisions. These limitations reinforce why tetanus remains a clinical diagnosis, though emerging technologies may eventually improve diagnostic capabilities, particularly for atypical presentations.
While tetanus diagnosis remains primarily clinical, modern laboratory tools are transforming management by enabling targeted prophylaxis, rapid risk assessment, and precision therapeutics. These strategies bridge critical gaps in wound care and immunity evaluation, particularly for high-risk cases.
Antitoxin Titer Kits
Rapid ELISA-based kits quantify tetanus antibody levels, guiding immunoglobulin prophylaxis and vaccine decisions within hours. Ideal for emergency departments evaluating wound exposure in patients with uncertain vaccination history.
Rapid Toxin Detection Assays
Experimental biosensors (e.g., lateral flow devices) detect tetanospasmin in wounds within 30 minutes—a potential game-changer for early confirmation in atypical cases, though still under validation.
Point-of-Care Wound Risk Stratification Tools
Algorithm-driven platforms integrate wound characteristics (depth/contamination) with patient immunity status to classify tetanus-prone wounds, standardizing triage and preventing unnecessary interventions.
Multiplex PCR for Wound Pathogens
Simultaneously identifies C. tetani (low sensitivity) and co-infecting bacteria (e.g., S. pyogenes), optimizing antibiotic selection while ruling out other causes of necrotizing wounds.
Despite advances in clinical awareness and supportive care, tetanus diagnostics continue to face significant hurdles, primarily due to the lack of reliable confirmatory tests and the time-sensitive nature of the disease. Future innovations, such as nanosensor-based tetanospasmin assays and host-response biomarker panels, hold promise for bridging this diagnostic gap. Additionally, global efforts to improve vaccination tracking could reduce clinical uncertainty in wound management.
Alta DiagnoTech provides comprehensive IVD solutions for tetanus diagnosis and prevention, including rapid antitoxin titer tests, wound pathogen detection kits, and emerging toxin biosensors, supporting clinical decision-making from initial suspicion to treatment monitoring. If you have related needs, please feel free to contact us for more information or product support.
Reference
This article is for research use only. Do not use in any diagnostic or therapeutic application.
|
There is no product in your cart. |