- Home
- Resource
- Disease Diagnosis
- Cancers
- Standardized Diagnostic Pathway for Prostate Cancer: From PSA Screening to Precise Stratification
- Home
- IVD
- By Technology Types
- By Diseases Types
- By Product Types
- Research
- Resource
- Distributors
- Company
Prostate cancer is a prevalent malignancy requiring a sophisticated diagnostic approach to balance early detection with personalized risk management. This resource provides a comprehensive guide to the standardized diagnostic pathway, detailing the integration of initial PSA screening, confirmatory biopsy, and advanced stratification tools that enable clinicians to distinguish between indolent and aggressive disease forms for optimal treatment decisions.
Prostate cancer is one of the most common cancers affecting men worldwide, characterized by the uncontrolled growth of abnormal cells in the prostate gland—a small walnut-shaped organ that produces seminal fluid. While many prostate cancers grow slowly and may remain confined to the prostate gland, others can be aggressive and spread rapidly. Diagnosis typically involves a multi-step approach beginning with prostate-specific antigen (PSA) blood testing and digital rectal exam (DRE), followed by biopsy confirmation and advanced imaging and biomarker tests for precise risk stratification and treatment planning.
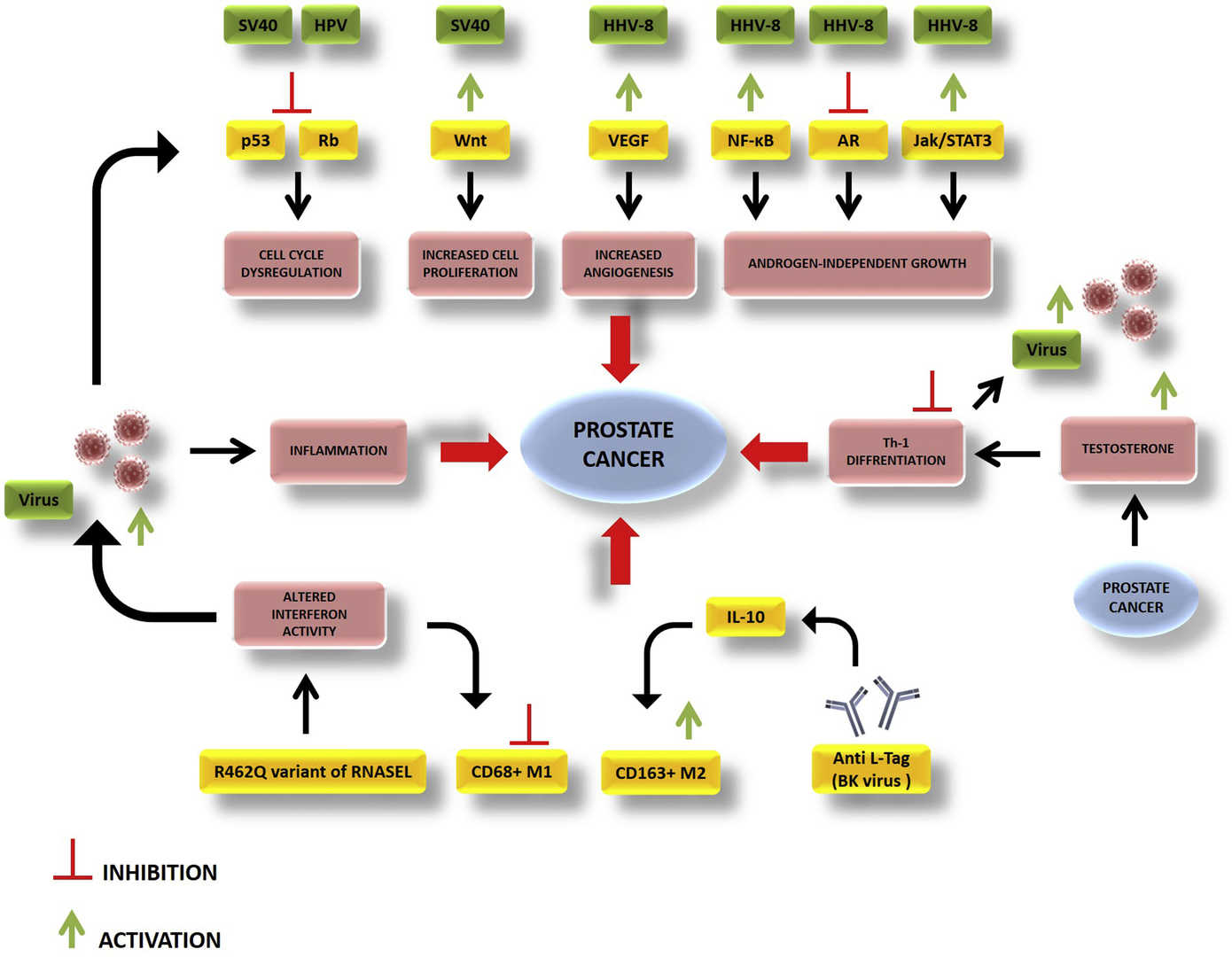 Fig.1 The interplay between host genetics, host immunity and viral infection that leads to initiation or promotion of prostate cancer. (Abidi, et al., 2018)
Fig.1 The interplay between host genetics, host immunity and viral infection that leads to initiation or promotion of prostate cancer. (Abidi, et al., 2018)
The diagnostic pathway for prostate cancer begins with non-invasive initial screening methods designed to identify individuals at elevated risk who require further investigation. These foundational tests serve as the critical first filter, triggering more definitive diagnostic procedures when results are abnormal. The two cornerstone components of this initial assessment are the prostate-specific antigen (PSA) blood test and the digital rectal exam (DRE).

The PSA test measures the blood level of a protein produced by both normal and malignant prostate cells, serving as the primary biochemical screening tool for prostate cancer. While an elevated PSA level can indicate the presence of cancer, it is not cancer-specific, as levels can also be increased by benign conditions such as prostatitis and benign prostatic hyperplasia (BPH). Clinical interpretation often considers not just the absolute PSA value but also factors like PSA velocity (rate of change over time), PSA density (PSA level relative to prostate volume), and the ratio of free-to-total PSA to improve diagnostic specificity.

The digital rectal exam is a physical examination in which a healthcare provider physically palpates the prostate gland through the rectal wall to assess its size, shape, and texture. The exam focuses on detecting palpable abnormalities such as firm areas, nodules, or asymmetry that might suggest malignancy. While the DRE has limitations in detecting cancers that are small or located in non-palpable areas of the prostate, it provides valuable complementary information to the PSA test, and an abnormality in either test typically warrants further diagnostic evaluation.
When initial screening tests suggest possible prostate cancer, the definitive diagnostic procedure is the prostate biopsy with subsequent pathological examination. This combined approach provides the conclusive evidence required for a cancer diagnosis by obtaining physical tissue samples for microscopic analysis. The process consists of two critical components: the biopsy procedure itself and the laboratory evaluation of the obtained tissue.
Prostate Biopsy
A prostate biopsy is typically performed as a transrectal ultrasound (TRUS)-guided procedure where a urologist uses a thin needle to obtain multiple small tissue cores (usually 10-12) from systematic areas of the prostate gland. This sampling method ensures adequate representation of the prostate tissue while minimizing patient discomfort. The procedure typically takes 20-30 minutes and is performed under local anesthesia with antibiotic prophylaxis to prevent infection.

Pathological Evaluation
The tissue cores obtained during biopsy undergo comprehensive pathological analysis to determine the presence, extent, and aggressiveness of cancer cells. This evaluation generates the Gleason score, which quantifies cancer aggressiveness by assessing cellular patterns on a scale of 1-5 across two dominant areas, with the combined score (ranging 2-10) forming the basis for grade groups (1-5) that correlate with disease prognosis and guide treatment decisions.
Following a prostate cancer diagnosis, modern medicine employs sophisticated tools to precisely determine the disease's aggressiveness and potential for progression, moving beyond basic detection to personalized risk assessment. These advanced methodologies provide crucial prognostic information that helps distinguish between indolent cancers suitable for active surveillance and aggressive diseases requiring immediate intervention, ultimately guiding tailored treatment decisions.
Advanced Biomarker Tests
These specialized molecular assays analyze unique genetic, protein, or cellular signatures in blood, urine, or tissue samples to provide enhanced prognostic information beyond traditional PSA testing. Tests such as the 4Kscore, Prostate Health Index (PHI), and Decipher Genomic Classifier evaluate specific biomarkers associated with cancer aggressiveness, helping clinicians predict the likelihood of significant disease progression and make more informed management decisions.
Advanced Imaging
Multiparametric magnetic resonance imaging (mpMRI) and PSMA-PET scans represent revolutionary imaging technologies that provide detailed visualization of prostate structure and cancer characteristics. mpMRI combines multiple imaging sequences to identify suspicious lesions and guide targeted biopsies, while PSMA-PET scanning utilizes prostate-specific membrane antigen targeting to detect metastatic spread with exceptional sensitivity, significantly improving staging accuracy and treatment planning.
Alta DiagnoTech provides a comprehensive portfolio of in vitro diagnostic (IVD) solutions supporting the complete prostate cancer care pathway. Our integrated product line enables healthcare providers to implement a standardized diagnostic approach, from initial risk assessment through precise stratification, with reliable, clinically-validated tools for improved patient management. If you have related needs, please feel free to contact us for more information or product support.
| Product Name | Technology | Application |
| Total PSA & Free PSA Assay Kit | Chemiluminescence Immunoassay (CLIA) | Initial prostate cancer screening and risk assessment through quantitative measurement of serum prostate-specific antigen |
| Prostate Health Index (PHI) Calculation Panel | Multiparametric Immunoassay with Algorithmic Analysis | Improved specificity for detecting clinically significant prostate cancer by combining total PSA, free PSA and [-2]proPSA measurements |
| Ultra-Sensitive PSA Monitoring Assay | High-Sensitivity Chemiluminescence Technology | Early detection of biochemical recurrence during post-treatment surveillance with detection limit <0.01 ng/mL |
Reference
This article is for research use only. Do not use in any diagnostic or therapeutic application.
|
There is no product in your cart. |