- Home
- Resource
- Disease Diagnosis
- Autoimmune Diseases
- Predicting the Path: Prognostic Serology in Systemic Sclerosis
- Home
- IVD
- By Technology Types
- By Diseases Types
- By Product Types
- Research
- Resource
- Distributors
- Company
Systemic sclerosis (scleroderma) is a complex autoimmune disorder characterized by vascular dysfunction, fibrosis, and heterogeneous organ involvement, making early and accurate diagnosis critical for mitigating severe complications. This resource explores how modern diagnostics, particularly prognostic serology, integrate with clinical evaluation and instrumental tools to stratify disease subtypes, predict organ-specific risks (e.g., ILD, PAH), and guide personalized management.
Systemic sclerosis (SSc), also known as scleroderma, is a rare and complex autoimmune disorder characterized by dysregulated fibrosis of the skin and internal organs, microvascular dysfunction, and aberrant immune activation. Its clinical presentation is highly heterogeneous, ranging from limited cutaneous involvement with slow progression to diffuse forms with rapid skin thickening and severe organ complications such as interstitial lung disease (ILD), pulmonary arterial hypertension (PAH), and scleroderma renal crisis. Diagnosis relies on integrating clinical features with specific autoantibody profiles (e.g., anti-centromere, anti-Scl-70, anti-RNA polymerase III), which are critical not only for confirmation but also for predicting disease subtype and prognostic outcomes.
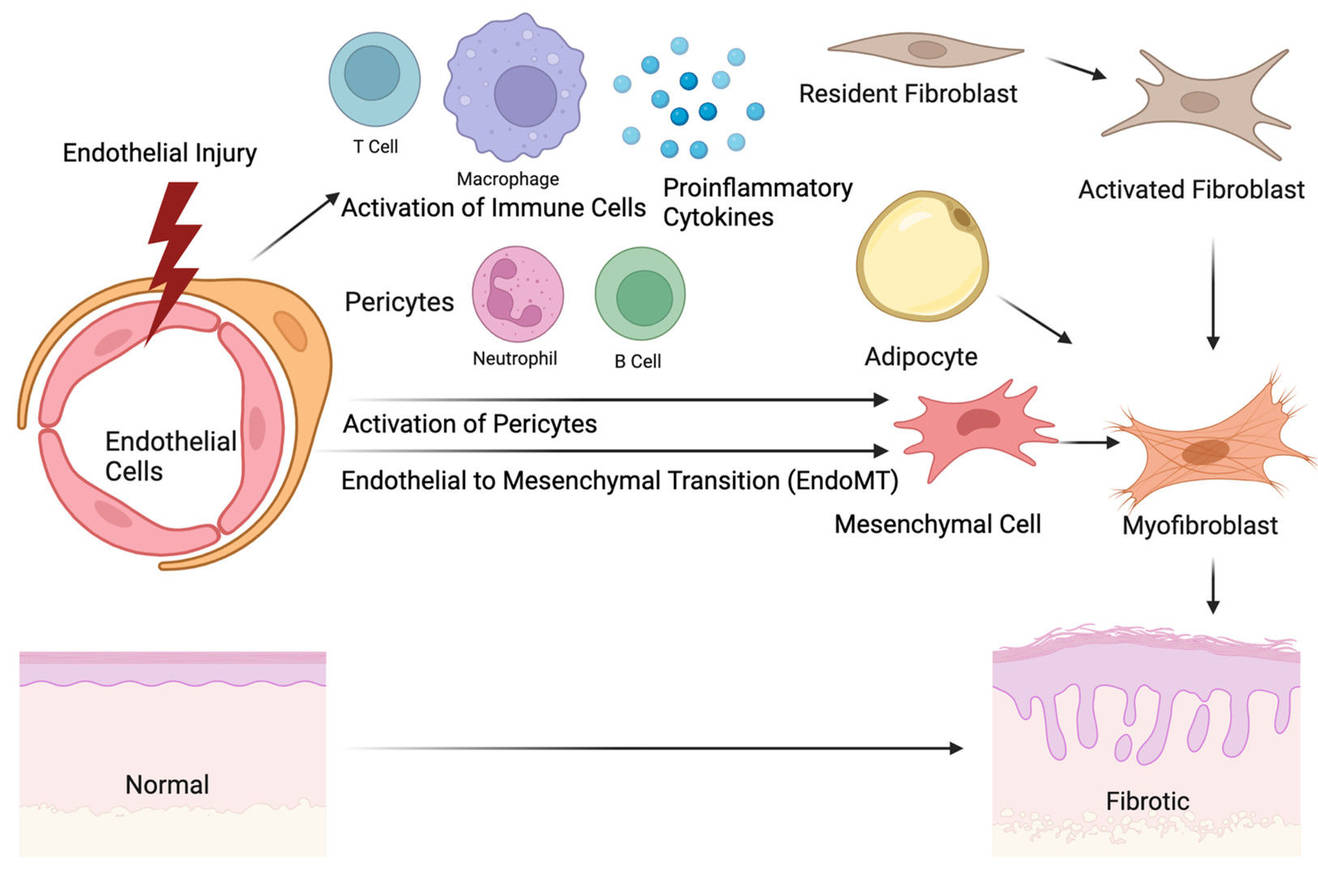 Fig.1 The origin of skin fibrosis in systemic sclerosis. (Ko J, et al., 2023)
Fig.1 The origin of skin fibrosis in systemic sclerosis. (Ko J, et al., 2023)

Clinical suspicion for systemic sclerosis (SSc) arises when patients present with characteristic triad of symptoms: Raynaud’s phenomenon (often severe and asymmetric), skin thickening (sclerodactyly progressing to broader fibrosis), and gastroesophageal reflux disease (GERD). Additional clues include digital ulcers, telangiectasias, calcinosis, and early symptoms of organ involvement such as dyspnea (suggesting ILD) or poorly controlled hypertension (hinting renal crisis). These findings, particularly in combination, should prompt immediate serological testing and specialist referral to confirm diagnosis and assess prognosis.
In systemic sclerosis (SSc), autoantibodies serve as highly specific serological biomarkers that are integral to diagnosis, classification, and prognostication. Unlike many autoimmune diseases, specific SSc-associated autoantibodies are often mutually exclusive and correlate strongly with distinct clinical phenotypes and organ involvement risks. Their detection provides critical insights beyond mere diagnosis, enabling early risk stratification and guiding personalized monitoring strategies. The most clinically significant autoantibodies include:
Anti-Topoisomerase I (Anti-Scl-70)
Highly specific for the diffuse cutaneous (dcSSc) subtype. Its presence confers a significantly elevated risk of progressive interstitial lung disease (ILD) and is associated with more severe skin involvement and higher mortality.
Anti-Centromere Antibody (ACA)
Primarily linked to the limited cutaneous (lcSSc) subtype. Patients with ACA are at increased risk for pulmonary arterial hypertension (PAH) and ischemic digital complications but have a lower likelihood of severe ILD or renal crisis.

Anti-RNA Polymerase III (Anti-RNAP3)
Strongly associated with rapid-onset skin thickening and the dcSSc subtype. This antibody carries the highest risk for scleroderma renal crisis and is also linked to an elevated risk of concurrent gastric cancer.
Other Prognostic Antibodies
The diagnosis and prognostication of systemic sclerosis (SSc) rely on a multimodal approach where serology acts as a pivotal guide, but rarely a standalone verdict. Integrating autoantibody profiles with other diagnostic tools is essential to confirm suspicion, assess organ involvement, and establish a baseline for monitoring. This synergy transforms individual test results into a powerful, cohesive clinical narrative.
Nailfold capillaroscopy visualizes early microvascular damage (e.g., giant capillaries, avascular areas), while serology (e.g., anti-centromere, anti-Scl-70) confirms diagnosis and subtypes. Their integration is critical for early detection, especially in patients with Raynaud’s phenomenon without overt fibrosis.
Serology guides targeted imaging: anti-Scl-70 mandates lung HRCT for interstitial disease, while anti-centromere prompts echocardiograms for pulmonary hypertension screening. This synergy ensures early intervention aligned with antibody-specific risks.
Serology defines baseline risk, while dynamic biomarkers (e.g., KL-6 for lung fibrosis, NT-proBNP for cardiac strain) monitor real-time organ activity. Combining both enables proactive management of disease flares and treatment response.
The future of prognostic serology lies in moving beyond traditional autoantibodies toward multiplex profiling and novel biomarkers (e.g., anti-angiogenic, chemokine, or epigenetic markers), integrated with artificial intelligence for pattern recognition. These advances aim to predict disease onset in pre-symptomatic individuals, refine organ-specific risk stratification beyond current antibodies, and dynamically monitor treatment response, ultimately enabling preemptive interventions and personalized therapeutic strategies.
Leveraging cutting-edge technology, Alta DiagnoTech delivers a comprehensive suite of IVD solution for systemic sclerosis, encompassing high-precision assay kits, advanced instrumentation, and dedicated consumables to support every step of the diagnostic journey. If you have related needs, please feel free to contact us for more information or product support.
Reference
| Cat.No | Product Name | Price |
|---|---|---|
| EK-YJL-1447 | Human RNA Polymerase III (Pol III) Antibody ELISA Kit | Add To Cart |
| EC-0071 | Human IL-17A ELISA Kit | Add To Cart |
| EC-0065 | Human IL-10 HS ELISA Kit | Add To Cart |
| IP-00189 | Influenza A rapid assay kit | Add To Cart |
| EC-0021 | Murine VEGF-A ELISA Kit | Add To Cart |
| EC-0072 | Human IP-10 ELISA Kit | Add To Cart |
| EC-003 | Human VEGF R1 ELISA Kit | Add To Cart |
| EC-0064 | Human IL-2 HS ELISA Kit | Add To Cart |
| CA-00162 | Typhoid IgG/IgM rapid assay kit | Add To Cart |
| CA-00153 | Chagas rapid assay kit | Add To Cart |
| IP-00175 | Legionella pneumophila rapid assay kit | Add To Cart |
| EC-0047 | Human CD124 ELISA Kit | Add To Cart |
| IP-00195 | Influenza H1N1 combo rapid assay kit | Add To Cart |
This article is for research use only. Do not use in any diagnostic or therapeutic application.
|
There is no product in your cart. |