Amyotrophic lateral sclerosis (ALS) presents significant diagnostic challenges, with current delays averaging 12-14 months from symptom onset. This resource explores cutting-edge advancements in ALS diagnostics, from emerging biomarkers to imaging & electrophysiology and genetic testing, highlighting how integrated IVD solutions can overcome current diagnostic challenges and enable earlier, more precise detection of this complex neurodegenerative disease.
Introduction to Amyotrophic Lateral Sclerosis (ALS)
Amyotrophic lateral sclerosis (ALS) is a progressive and fatal neurodegenerative disorder characterized by the degeneration of motor neurons, leading to muscle weakness, paralysis, and eventual respiratory failure. With no definitive diagnostic test currently available, ALS diagnosis relies on clinical assessments, electrophysiological studies, and the exclusion of mimic disorders, often resulting in delays of 12–14 months from symptom onset. Emerging biomarkers, such as neurofilament light chain (NfL) and TDP-43 aggregates, alongside genetic testing for mutations in SOD1, C9ORF72, and other genes, are transforming the diagnostic landscape.
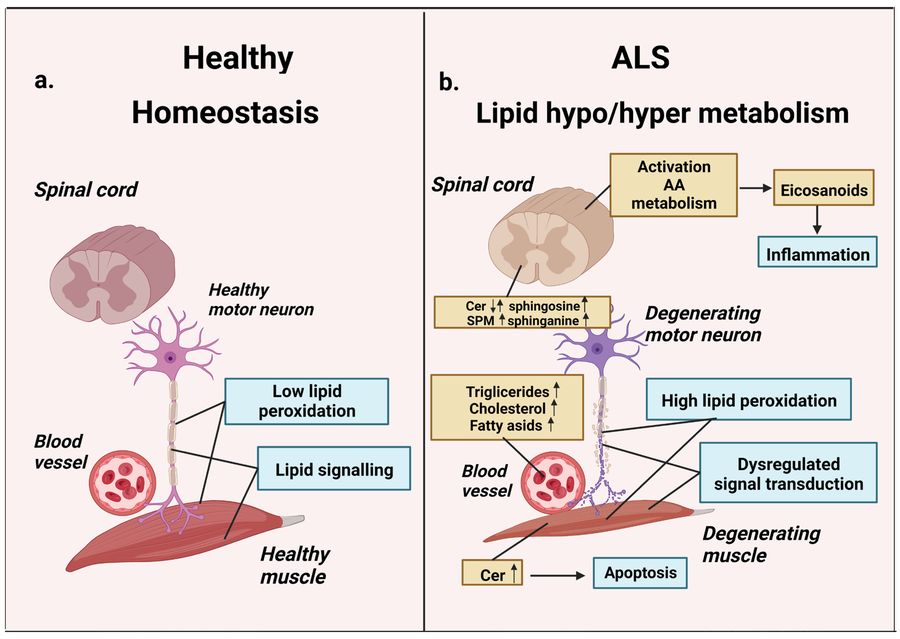 Fig.1 Lipid metabolism in homeostasis and amyotrophic lateral sclerosis (ALS). (Alessenko A V, et al., 2023)
Fig.1 Lipid metabolism in homeostasis and amyotrophic lateral sclerosis (ALS). (Alessenko A V, et al., 2023)
Biomarkers for Amyotrophic Lateral Sclerosis (ALS) Diagnosis
Amyotrophic lateral sclerosis (ALS) lacks a single definitive diagnostic test, making biomarker discovery critical for early detection, differential diagnosis, and disease monitoring. Recent advances highlight several promising candidates:
Neurofilament Light Chain (NfL)
A key biomarker of axonal damage, NfL is significantly elevated in the CSF and serum of ALS patients, correlating with disease progression and survival. While highly sensitive for neurodegeneration, its lack of specificity necessitates integration with clinical findings.
TDP-43 Aggregates
The pathological hallmark of ALS, TDP-43 mislocalization and aggregation occurs in >97% of cases. Though traditionally detected post-mortem, emerging CSF exosome assays and seed amplification techniques aim to identify TDP-43 abnormalities pre-mortem.
Tau Protein
While primarily linked to Alzheimer's, phosphorylated tau (p-tau) shows modest elevation in ALS CSF, potentially reflecting comorbid pathologies or secondary neurodegeneration. Its utility lies in differential diagnosis, though it lacks standalone diagnostic value for ALS.
Imaging & Electrophysiology in Amyotrophic Lateral Sclerosis (ALS) Diagnosis
Imaging and electrophysiology play critical roles in amyotrophic lateral sclerosis (ALS) diagnosis by objectively detecting upper and lower motor neuron degeneration, supporting clinical evaluation when symptoms are ambiguous. These tools help differentiate ALS from mimics, track disease progression, and provide biomarkers for clinical trials. While not standalone diagnostic methods, they significantly enhance diagnostic confidence when combined with clinical and fluid biomarker findings.
Imaging in ALS
Advanced MRI techniques (e.g., diffusion tensor imaging [DTI], voxel-based morphometry) reveal corticospinal tract degeneration, motor cortex thinning, and metabolic changes, while PET imaging (e.g., TSPO tracers for neuroinflammation) provides functional insights. Though not yet routine, these methods improve early detection and differential diagnosis.
Electrophysiology in ALS
Electromyography (EMG) remains the gold standard for detecting lower motor neuron (LMN) dysfunction, while transcranial magnetic stimulation (TMS) assesses upper motor neuron (UMN) impairment. Emerging techniques like high-density EMG and electrical impedance myography (EIM) enhance sensitivity for early ALS diagnosis and longitudinal monitoring.
Genetic Testing in Amyotrophic Lateral Sclerosis (ALS)
Genetic testing is essential for diagnosing familial amyotrophic lateral sclerosis (ALS), clarifying sporadic cases, and guiding personalized treatment. By identifying pathogenic mutations in ALS-associated genes, it enables early intervention, family risk assessment, and eligibility for gene-specific therapies. While only 10–15% of ALS cases are familial, genetic testing reveals causative mutations in 5–10% of sporadic patients, making it a critical tool for precision medicine in ALS.
Major ALS-Associated Genes
- C9ORF72 (40% of familial ALS): GGGGCC repeat expansions – linked to ALS-FTD spectrum.
- SOD1 (15%): Missense mutations (e.g., A4V, D90A) with varying progression rates.
- FUS/TARDBP (5% each): Disrupt RNA processing and TDP-43 pathology.
- Emerging genes (TBK1, NEK1, OPTN): Implicated in autophagy and neuroinflammation.
Testing Methodologies
- Targeted NGS Panels: Cost-effective for screening 30+ ALS genes (e.g., C9ORF72, SOD1).
- Repeat Expansion Analysis: Specialized PCR/capillary electrophoresis for C9ORF72.
- Whole-Exome Sequencing (WES): For atypical cases or research (identifies novel variants).
The Future of Amyotrophic Lateral Sclerosis (ALS) Diagnostics
The future of amyotrophic lateral sclerosis (ALS) diagnostics is moving toward pre-symptomatic detection and precision medicine, driven by advances in multi-omics profiling, ultra-sensitive biomarkers, and AI-powered analysis. Emerging technologies like single-molecule assays, liquid biopsies, and advanced neuroimaging aim to reduce diagnostic delays. Genetic testing will expand with polygenic risk scores, while wearable sensors and digital biomarkers may enable real-time monitoring.
Alta DiagnoTech offers comprehensive IVD products for amyotrophic lateral sclerosis (ALS), including cutting-edge biomarker test kits and genetic testing systems to accelerate and improve ALS testing worldwide. If you have related needs, please feel free to contact us for more information or product support.
Reference
- Alessenko A V, Gutner U A, Shupik M A. Involvement of lipids in the pathogenesis of amyotrophic lateral sclerosis[J]. Life, 2023, 13(2): 510.
This article is for research use only. Do not use in any diagnostic or therapeutic application.



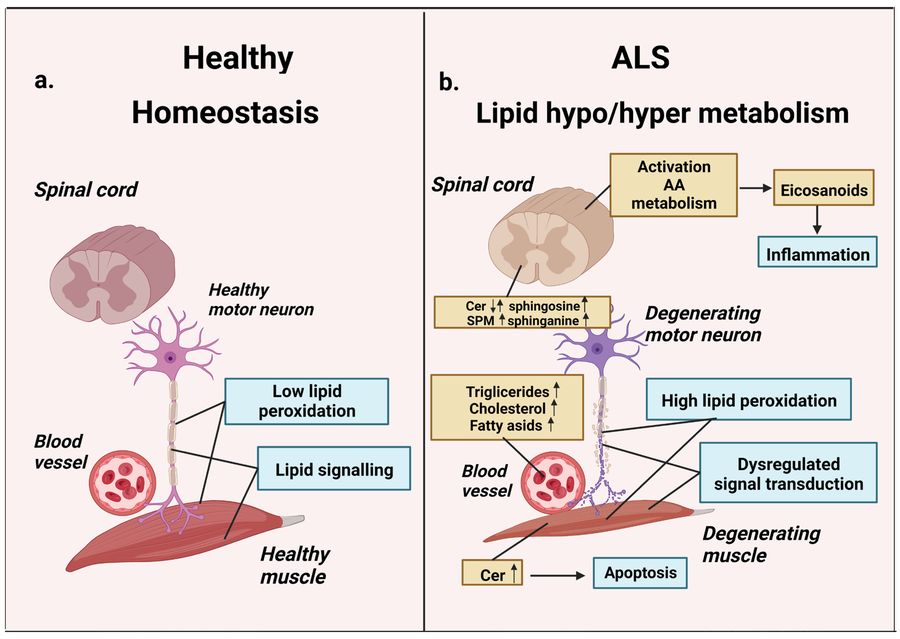 Fig.1 Lipid metabolism in homeostasis and amyotrophic lateral sclerosis (ALS). (Alessenko A V, et al., 2023)
Fig.1 Lipid metabolism in homeostasis and amyotrophic lateral sclerosis (ALS). (Alessenko A V, et al., 2023)