- Home
- Resource
- Disease Diagnosis
- Endocrine Diseases
- From Suspicion to Confirmation: Mapping the Diagnostic Pathway for Hypopituitarism
- Home
- IVD
- By Technology Types
- By Diseases Types
- By Product Types
- Research
- Resource
- Distributors
- Company
Hypopituitarism is defined by deficient secretion of one or more pituitary hormones. This resource outlines the structured diagnostic pathway for this condition, beginning with the initial clinical and biochemical evaluation. It details the critical process of dynamic hormone axis testing and concludes with the synthesis of findings for definitive diagnosis. An overview of the relevant in vitro diagnostic (IVD) solutions supporting this pathway is also provided.
Hypopituitarism is a clinical syndrome characterized by the partial or complete deficiency of one or more hormones produced by the anterior or posterior pituitary gland. This deficiency results from the impaired function of the pituitary itself or its connection to the hypothalamus, leading to a wide spectrum of non-specific symptoms—such as chronic fatigue, unexplained weight changes, sexual dysfunction, and hypotension—that often mimic other conditions. The most critical and potentially life-threatening deficiency is that of the adrenocorticotropic hormone (ACTH), which can precipitate an adrenal crisis. Therefore, a systematic diagnostic approach, beginning with the evaluation of the hypothalamic-pituitary-adrenal (HPA) axis, is essential to identify the specific hormonal deficits, determine the underlying etiology (e.g., tumor, infarction, genetic disorder), and initiate appropriate, life-sustaining hormone replacement therapy.
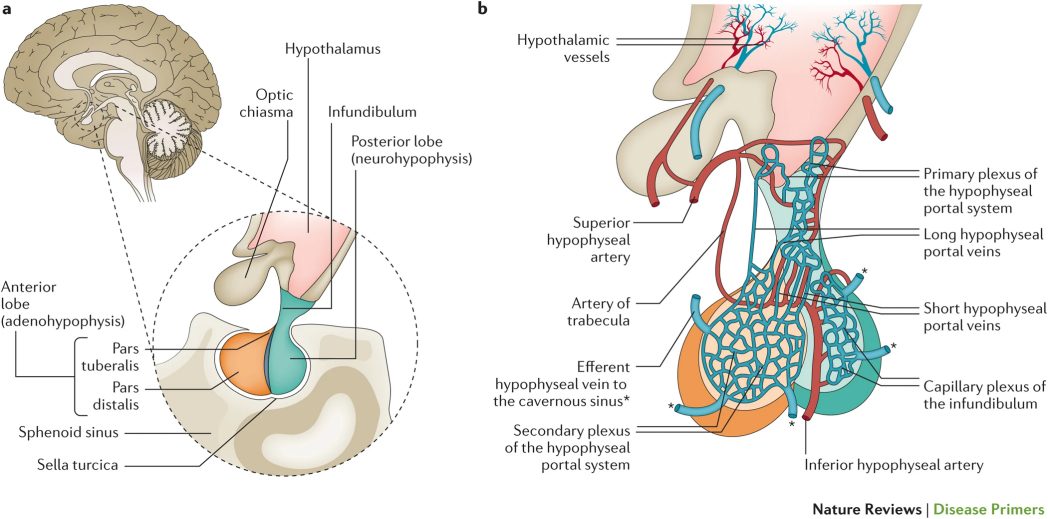 Fig.1 Anatomy and vascularization of the pituitary gland. (Karaca Z, et al., 2016)
Fig.1 Anatomy and vascularization of the pituitary gland. (Karaca Z, et al., 2016)
The diagnostic journey for hypopituitarism begins with clinical suspicion, triggered by recognizing patterns of non-specific symptoms—such as profound fatigue, unexplained weight loss, cold intolerance, loss of libido, or failure to thrive in children—that may reflect deficiencies across one or multiple hormone axes. A thorough history is paramount, focusing on "red flags" like headaches or visual disturbances (suggesting a pituitary mass), a history of pituitary surgery or cranial radiation, and specific events such as postpartum hemorrhage (Sheehan's syndrome). The initial baseline laboratory evaluation strategically includes morning serum cortisol and free thyroxine (FT4), as deficiencies in the adrenal and thyroid axes carry the highest acute risk, while simultaneous pituitary MRI is essential to identify structural abnormalities and establish an anatomical cause for the suspected hormonal dysfunction. This combined clinical, biochemical, and radiological approach forms the critical foundation upon which targeted dynamic hormone testing is built.
The diagnosis of hypopituitarism requires more than baseline hormone measurements; it necessitates dynamic functional testing to accurately assess the reserve capacity of each pituitary axis. Due to the hierarchical nature of pituitary control and the life-threatening nature of certain deficiencies, this evaluation must follow a systematic, prioritized sequence. This section details the key provocative and stimulation tests that are essential for confirming hormone deficiencies and guiding safe replacement therapy.
Assessment of the HPA (ACTH-Cortisol) Axis
This is the first and most critical axis to evaluate, as untreated central adrenal insufficiency can be fatal. The gold-standard test is the insulin tolerance test (ITT), which induces hypoglycemia to maximally stimulate ACTH and cortisol release. Due to its risks, safer alternatives like the ACTH stimulation test (standard or low-dose) are often used first-line, though they may miss recent-onset secondary deficiency. The metyrapone test is another option to assess the integrity of the entire hypothalamic-pituitary-adrenal (HPA) axis.

Assessment of the Thyroid (TSH-T4) Axis
Central hypothyroidism is diagnosed biochemically by finding a low free T4 (FT4) level with a low or inappropriately normal TSH. Dynamic testing is typically not required for diagnosis, making it a straightforward assessment once the HPA axis is secured. However, it is crucial to evaluate this axis only after confirming sufficient cortisol replacement or HPA axis integrity, as treating hypothyroidism in a patient with untreated adrenal insufficiency can precipitate an adrenal crisis.

Assessment of the Gonadal (LH/FSH-Sex Hormones) Axis
Evaluation involves measuring LH, FSH, and the relevant sex steroid (estradiol in women, testosterone in men). In premenopausal women, the menstrual history is a key functional indicator. In men and postmenopausal women, low sex steroids with inappropriately low or normal gonadotropins confirm the diagnosis. Dynamic testing (e.g., GnRH stimulation) is rarely necessary for clinical diagnosis but may be used in specific research or complex pediatric cases.

Assessment of the GH-IGF-1 Axis and Posterior Pituitary
Growth hormone (GH) deficiency is assessed by measuring IGF-1 as a screening marker. A low IGF-1 in the appropriate clinical context necessitates confirmation with a dynamic stimulation test, such as the GHRH + Arginine test or the ITT (if performed for the HPA axis). For the posterior pituitary, the diagnosis of central diabetes insipidus (DI) is primarily clinical (polyuria, polydipsia) and confirmed by the water deprivation test, which evaluates the kidney's ability to concentrate urine in response to endogenous or exogenous vasopressin.
After completing the systematic evaluation of individual hormone axes, the final and critical phase is to synthesize all findings into a definitive, actionable diagnosis. This step moves beyond isolated test results to integrate clinical context, dynamic testing data, and imaging, ensuring an accurate understanding of the extent and etiology of pituitary dysfunction. It also requires distinguishing hypopituitarism from other mimicking conditions and avoiding common interpretive errors.

This step synthesizes results from all hormone axes to define the deficiency pattern—isolated or combined. Interpretation must follow a hierarchical order; for instance, confirm a functional ACTH-cortisol axis before reliably diagnosing central hypothyroidism, as cortisol deficiency can suppress TSH. Finally, correlate the biochemical profile with pituitary MRI findings to identify a structural cause.

The core task is distinguishing central (secondary) from primary gland failure by analyzing pituitary trophic hormone patterns. Key pitfalls to avoid include: over-relying on a single random cortisol level, mistaking central hypothyroidism (low FT4, low/normal TSH) for non-thyroidal illness, and initiating thyroid hormone replacement before securing adrenal axis sufficiency, which risks precipitating an adrenal crisis. A systematic, integrated approach is essential for accuracy and safety.
Alta DiagnoTech provides a comprehensive in vitro diagnostic (IVD) portfolio for hypopituitarism, supporting the complete diagnostic cascade from initial suspicion through dynamic axis confirmation. Our solutions encompass precise assays for both baseline hormone levels and critical components for stimulation tests, enabling clinicians to accurately evaluate the functional reserve of the pituitary gland. With reliable technologies ranging from automated immunoassays to advanced molecular testing, we empower laboratories to deliver the definitive data needed for safe diagnosis, appropriate hormone replacement, and improved patient outcomes. If you have related needs, please feel free to contact us for more information or product support.
| Product Name | Technology | Application |
| Cortisol CLIA Kit | Chemiluminescent Immunoassay (CLIA) | Quantification of serum cortisol levels for baseline assessment and as the key readout in dynamic tests (e.g., ACTH stimulation test, Insulin Tolerance Test). |
| ACTH CLIA Kit | Chemiluminescent Immunoassay (CLIA) | Measurement of plasma ACTH to help differentiate primary from secondary adrenal insufficiency. |
| Free T4 (FT4) & TSH CLIA Kits | Chemiluminescent Immunoassay (CLIA) | Essential duo for evaluating the thyroid axis. A low FT4 with a low/normal TSH is diagnostic for central hypothyroidism. |
| LH & FSH CLIA Kits | Chemiluminescent Immunoassay (CLIA) | Measurement of gonadotropins alongside sex steroids (estradiol, testosterone) for assessing the gonadal axis. |
| IGF-1 CLIA Kit | Chemiluminescent Immunoassay (CLIA) | Screening marker for Growth Hormone (GH) deficiency; a low IGF-1 prompts further dynamic GH testing. |
| Cosyntropin (ACTH 1-24) for Injection | Synthetic Peptide | The diagnostic agent used for the standard and low-dose ACTH stimulation test to assess adrenal reserve. |
| Pituitary Hormone Deficiency NGS Panel | Next-Generation Sequencing (NGS) | Genetic analysis to identify mutations associated with congenital or familial forms of hypopituitarism. |
Reference
This article is for research use only. Do not use in any diagnostic or therapeutic application.
|
There is no product in your cart. |