- Home
- Resource
- Disease Diagnosis
- Cardiovascular Diseases
- Efficiency in Heart Failure Diagnosis: Leveraging Biomarkers for Faster, Accurate Results
- Home
- IVD
- By Technology Types
- By Diseases Types
- By Product Types
- Research
- Resource
- Distributors
- Company
Heart failure is a complex clinical syndrome where the heart's ability to pump blood is compromised, leading to debilitating symptoms like breathlessness and fatigue. This resource page provides a comprehensive overview of the modern, biomarker-driven approach to diagnosing this condition. The following sections will detail the foundational and emerging biomarker landscape, illustrate their tangible impact on clinical pathways, and highlight the advanced diagnostic solutions that support this modern paradigm.
Heart failure (HF) is a complex clinical syndrome characterized by the heart's inability to pump blood effectively to meet the body's metabolic demands. It results from any structural or functional impairment of ventricular filling or ejection of blood. Rather than implying the heart has stopped working, the term signifies a state of inadequate cardiac output, often leading to symptoms such as breathlessness, fatigue, fluid retention (edema), and reduced exercise capacity. These hallmark symptoms arise from underlying conditions like coronary artery disease, hypertension, or cardiomyopathies, which trigger neurohormonal activation and pathological remodeling of the heart, creating a progressive cycle of functional decline.
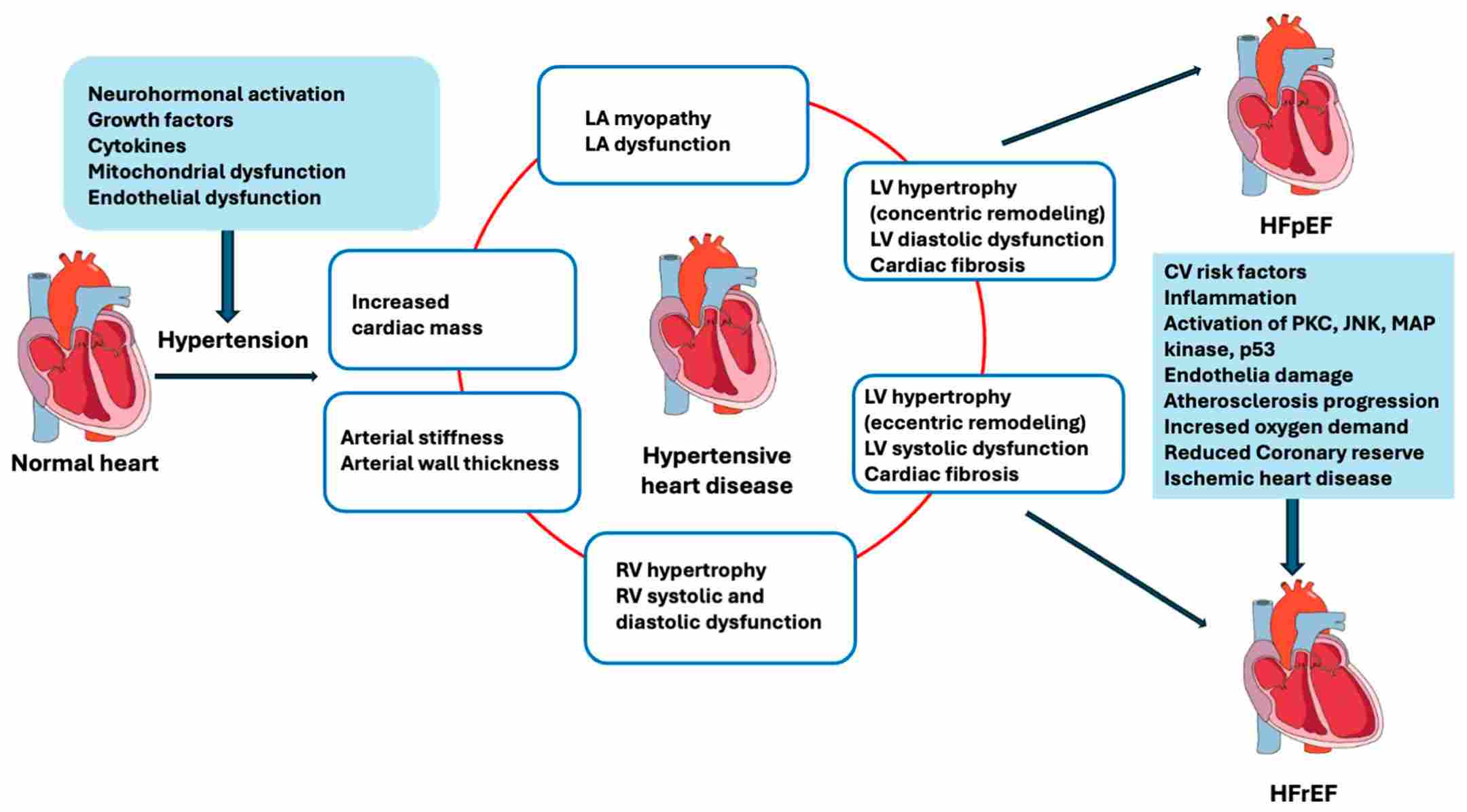 Fig.1 Progression from hypertension to heart failure (HF). (Gallo G, Savoia C., 2024)
Fig.1 Progression from hypertension to heart failure (HF). (Gallo G, Savoia C., 2024)
The accurate and timely diagnosis of heart failure is often challenged by the non-specific nature of its symptoms. This is where biomarker testing becomes indispensable, providing an objective, quantitative measure of cardiac stress and dysfunction to guide clinical decision-making. By integrating key biomarkers into the diagnostic workup, healthcare professionals can significantly improve efficiency, moving from suspicion to confirmation with greater speed and accuracy. At the very heart of this modern approach lie the cornerstone biomarkers: B-type natriuretic peptide (BNP) and its inactive counterpart, N-terminal pro-B-type natriuretic peptide (NT-proBNP).

B-type Natriuretic Peptide (BNP)
B-type natriuretic peptide (BNP) is a hormone primarily secreted by the cardiac ventricles in direct response to myocardial wall stress and volume overload. When measured in circulation, BNP levels provide a real-time snapshot of the heart's hemodynamic burden. Its key clinical utility lies in its exceptional negative predictive value; very low BNP levels make the diagnosis of acutely decompensated heart failure highly unlikely, effectively ruling out the condition and prompting the search for alternative causes of the patient's symptoms.
N-terminal pro-B-type Natriuretic Peptide (NT-proBNP)
N-terminal pro-B-type natriuretic peptide (NT-proBNP) is the inactive fragment co-released with BNP upon the cleavage of its pro-hormone. While physiologically linked, NT-proBNP has distinct analytical advantages, including a longer half-life and greater in-vitro stability, which can contribute to higher circulating levels and potentially enhanced sensitivity. Like BNP, it is central to the diagnostic algorithm for both acute and chronic heart failure, with established cut-off values that robustly aid in ruling out the disease, assessing its severity, and stratifying patient risk.
While natriuretic peptides (BNP and NT-proBNP) remain the cornerstone for diagnosis and prognosis, the heart failure biomarker landscape is rapidly expanding. Modern research focuses on a "multi-marker" strategy that reflects the complex, multifaceted nature of the HF syndrome. By measuring different biological pathways involved in myocardial injury, fibrosis, and inflammation, clinicians can move beyond simple diagnosis to gain a deeper understanding of disease severity, specific pathophysiology, and individualized patient risk. This approach allows for more precise prognostication and holds the promise of guiding targeted therapies in the future. The most prominent of these emerging biomarkers include:

A highly specific marker of myocardial injury. In the context of HF, persistently elevated hs-cTn indicates ongoing cardiomyocyte damage and is a powerful predictor of adverse outcomes, independent of natriuretic peptide levels. Its detection underscores the progressive nature of the disease.

This biomarker is involved in processes of cardiac fibrosis and remodeling. sST2 levels are strongly associated with an increased risk of mortality and hospitalization. A key advantage is that its concentration is not significantly affected by age, obesity, or renal function, making it a valuable complementary tool, especially for risk stratification in chronic HF.

A biomarker primarily expressed during macrophage activation and plays a key role in promoting cardiac inflammation and fibrosis. Elevated Gal-3 levels are linked to worse long-term outcomes and help identify patients with a progressive, fibrotic phenotype of HF, which may be less responsive to certain standard therapies.
The integration of biomarkers like BNP and NT-proBNP into heart failure pathways delivers measurable improvements across the care continuum. By providing objective, rapid results, they transform diagnostic workflows and patient management.
Alta DiagnoTech is dedicated to empowering healthcare professionals with a comprehensive and reliable portfolio of IVD solutions for heart failure. Our high-precision assays are designed to seamlessly integrate into your laboratory's workflow, providing the critical data needed to enhance diagnostic confidence, optimize patient management, and improve clinical outcomes across the heart failure continuum. If you have related needs, please feel free to contact us for more information or product support.
| Product Name | Technology | Application |
| NT-proBNP Assay Kit | Chemiluminescent Immunoassay (CLIA) | Quantitative measurement of NT-proBNP in human plasma for aid in diagnosis and risk stratification of heart failure. |
| BNP Assay Kit | Chemiluminescent Immunoassay (CLIA) | Quantitative measurement of BNP in human plasma for aid in diagnosis and monitoring of acute heart failure. |
| High-Sensitivity Troponin I Assay | Chemiluminescent Immunoassay (CLIA) | Highly precise quantitative detection of cardiac Troponin I for assessment of myocardial injury in heart failure patients. |
| sST2 Assay Kit | Enzyme-Linked Immunosorbent Assay (ELISA) | Quantitative measurement of soluble ST2 in human serum for prognostic risk stratification in chronic heart failure. |
| Galectin-3 Assay Kit | Chemiluminescent Immunoassay (CLIA) | Quantitative measurement of Galectin-3 in human plasma to aid in prognostic assessment of heart failure progression. |
Reference
This article is for research use only. Do not use in any diagnostic or therapeutic application.
|
There is no product in your cart. |