- Home
- Resource
- Disease Diagnosis
- Cancers
- Diagnosis of Small Cell Lung Cancer (SCLC): A Guide to Pathology and Biomarkers
- Home
- IVD
- By Technology Types
- By Diseases Types
- By Product Types
- Research
- Resource
- Distributors
- Company
Small cell lung cancer (SCLC) is an aggressive, high-grade neuroendocrine malignancy characterized by rapid growth and early, widespread metastasis. This resource provides a comprehensive guide to its diagnosis, detailing the critical diagnostic journey from clinical suspicion to pathological confirmation, with a focused exploration of the essential histopathological features and the definitive role of immunohistochemistry (IHC) and key biomarkers in establishing a precise diagnosis.
Small cell lung cancer (SCLC) is a highly aggressive, rapidly proliferating neuroendocrine malignancy, predominantly associated with a strong history of cigarette smoking. Accounting for approximately 10-15% of all lung cancers, SCLC is characterized by its early and widespread metastatic potential, with the majority of patients presenting with extensive-stage disease at diagnosis. Its clinical course is notably aggressive, featuring a high initial response rate to platinum-based chemotherapy and radiotherapy; however, the development of therapeutic resistance is common, leading to a dismal overall prognosis with a five-year survival rate that remains disappointingly low. This underscores the critical and urgent need for a rapid, accurate, and definitive pathological diagnosis to guide appropriate treatment strategies and patient management.
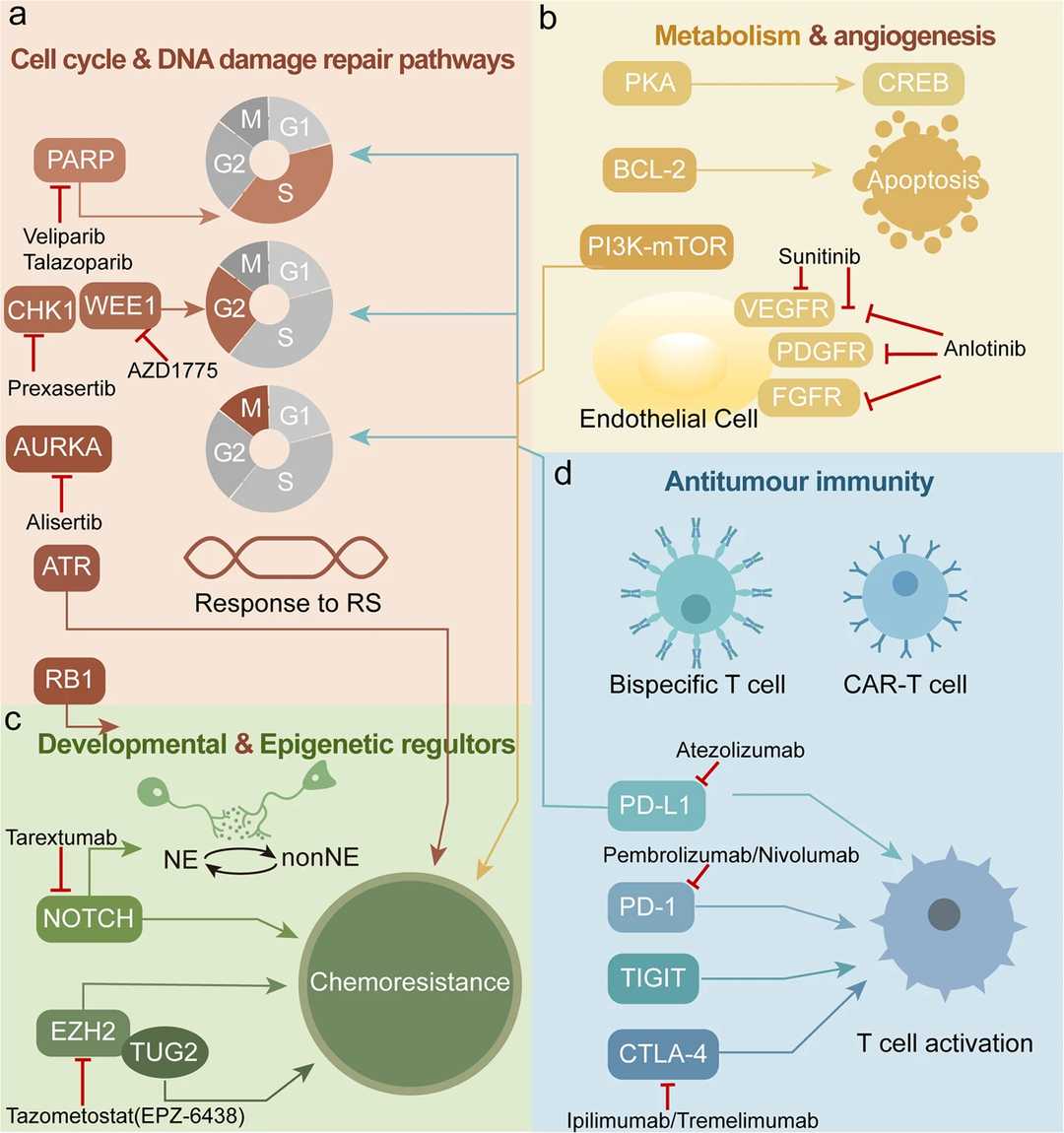 Fig.1 Six main representative therapeutically tractable targets in small-cell lung cancer (SCLC). (Yuan, Min, et al., 2022)
Fig.1 Six main representative therapeutically tractable targets in small-cell lung cancer (SCLC). (Yuan, Min, et al., 2022)
The diagnosis of small cell lung cancer (SCLC) is a rapid, multistep process, beginning with concerning clinical signs and culminating in a pathological diagnosis. This process typically begins with the patient's clinical presentation. Symptoms are often significant and include persistent cough, hemoptysis, dyspnea, and systemic effects of paraneoplastic syndromes, such as syndrome of inappropriate antidiuretic hormone secretion (SIADH) or Cushing's syndrome. This initial suspicion requires histological confirmation. The choice of biopsy method should be determined based on the patient's anatomy and the extent of disease. Commonly used methods include:
While clinical and radiological findings raise the suspicion of small cell lung cancer (SCLC), the definitive diagnosis rests unequivocally on the pathological examination of tissue. The initial and fundamental step in this process is the histopathological assessment of morphology—the study of the tissue's microscopic structure and the cellular appearance. This analysis, performed on hematoxylin and eosin (H&E) stained slides, forms the indispensable cornerstone upon which all further diagnostic testing is built. The classic morphological features of SCLC, as revealed under the microscope, are distinctive:
While histopathology provides the initial diagnostic clue, the inherent limitations of morphology often create a crossroads of uncertainty for the pathologist. It is at this critical juncture that immunohistochemistry (IHC) proves indispensable, transforming subjective interpretation into an objective, biomarker-driven diagnosis. IHC serves as the definitive tool to resolve diagnostic dilemmas, confirm the neuroendocrine nature of SCLC, and precisely distinguish it from a host of other malignancies with overlapping morphological features. A robust IHC work-up for SCLC relies on a core panel of well-characterized biomarkers:
Alta DiagnoTech is committed to empowering precise diagnosis in oncology by providing a comprehensive portfolio of high-quality in vitro diagnostic (IVD) products for small cell lung cancer (SCLC). Our solutions are specifically designed to support pathology laboratories in confirming diagnosis, differentiating SCLC from other malignancies, and providing critical prognostic insights. From robust immunohistochemistry (IHC) assays for key neuroendocrine biomarkers to advanced molecular tests, our products ensure accuracy, reliability, and confidence at every step of the diagnostic journey. If you have related needs, please feel free to contact us for more information or product support.
| Product Name | Technology | Application |
| CD56 (NCAM) IHC Assay Kit | Immunohistochemistry (IHC) | Detection of CD56 protein expression to aid in the identification of neuroendocrine differentiation; a highly sensitive marker for SCLC. |
| Synaptophysin IHC Detection Kit | Immunohistochemistry (IHC) | Detection of Synaptophysin protein expression to confirm the neuroendocrine lineage of tumors. |
| Chromogranin A IHC Kit | Immunohistochemistry (IHC) | Detection of Chromogranin A protein expression, providing high specificity for neuroendocrine tumors. |
| TTF-1 IHC Assay | Immunohistochemistry (IHC) | Detection of TTF-1 nuclear staining to support a pulmonary origin for the carcinoma and aid in differential diagnosis. |
| Ki-67 Proliferation Index IHC Kit | Immunohistochemistry (IHC) | Determination of tumor proliferation index; critical for differentiating high-grade SCLC (showing very high index) from lower-grade neuroendocrine tumors. |
| INSM1 IHC Assay Kit | Immunohistochemistry (IHC) | Detection of INSM1, a novel and highly sensitive nuclear biomarker for neuroendocrine neoplasms, useful in diagnostically challenging cases. |
| Pan-Cytokeratin IHC Cocktail | Immunohistochemistry (IHC) | Confirmation of epithelial origin, helping to distinguish SCLC from lymphomas (which are cytokeratin-negative). |
| SCLC Molecular Subtyping Panel | Next-Generation Sequencing (NGS) | Detection of key genomic alterations (e.g., in TP53, RB1) and RNA-based classifiers to identify SCLC molecular subtypes (SCLC-A, N, P, I) for research and prognostic purposes. |
Reference
This article is for research use only. Do not use in any diagnostic or therapeutic application.
|
There is no product in your cart. |