Rheumatic heart disease (RHD) is a preventable yet devastating chronic condition resulting from heart valve damage caused by acute rheumatic fever, an autoimmune response to a group A streptococcal infection. This resource provides a comprehensive guide to the modern diagnostic pathway for RHD, systematically exploring the integrated application of established clinical criteria, essential imaging technologies, critical laboratory testing, and the promising future of novel biomarkers to enable accurate detection and improved patient management.
Overview of Rheumatic Heart Disease
Rheumatic heart disease (RHD) is a chronic cardiovascular condition that results from permanent damage to the heart valves, primarily caused by an abnormal immune response to a preceding infection with group A streptococcus bacteria. This reaction, known as acute rheumatic fever (ARF), triggers inflammation that can lead to scarring of the heart valves, most commonly the mitral and aortic valves. Over time, this damage can cause valve stenosis or regurgitation, leading to heart failure, stroke, and premature death if left undiagnosed and untreated. RHD is a preventable yet persistent disease of poverty and health inequity, disproportionately affecting children and young adults in low-resource settings.
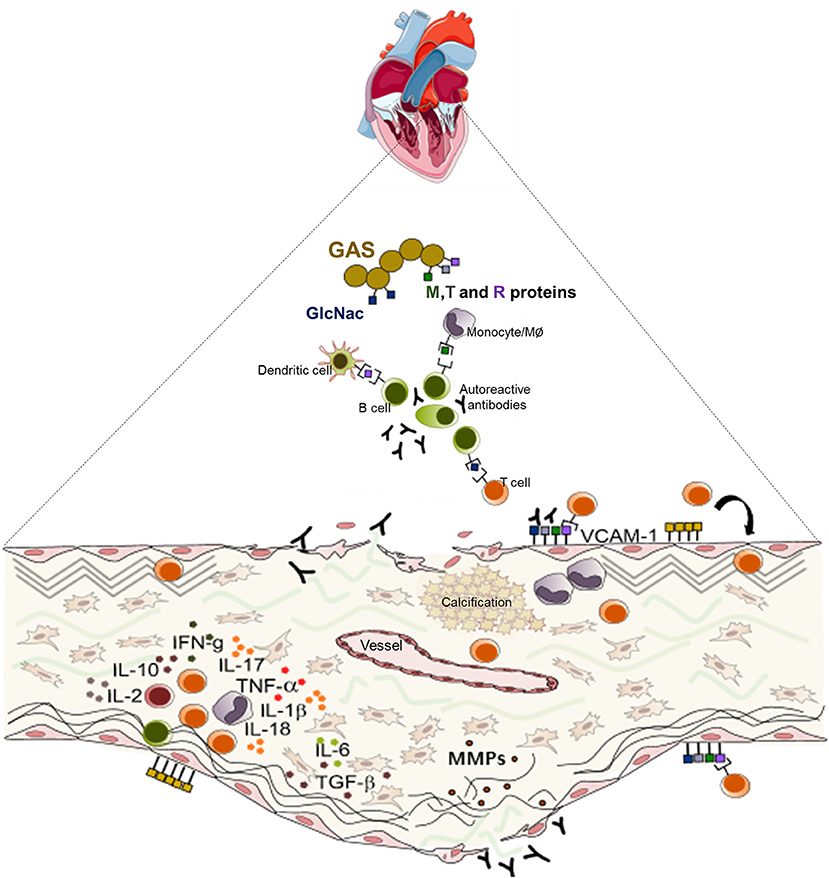 Fig.1 A schematic diagram illustrating the pathogenesis of rheumatic heart valve disease. (Passos L S A, et al., 2021)
Fig.1 A schematic diagram illustrating the pathogenesis of rheumatic heart valve disease. (Passos L S A, et al., 2021)
The Clinical Foundation: Understanding and Applying the Jones Criteria
The Jones criteria serve as the essential clinical foundation for diagnosing acute rheumatic fever (ARF), the precursor to rheumatic heart disease (RHD). This established guideline requires the presence of either two major manifestations or one major and two minor manifestations, plus laboratory evidence of a preceding group A streptococcal infection. The major criteria include carditis, arthritis, chorea, subcutaneous nodules, and erythema marginatum, while the minor criteria comprise clinical features like fever and arthralgia, alongside laboratory findings of elevated acute-phase reactants. Its application is crucial for initiating prompt treatment and secondary antibiotic prophylaxis to prevent the development of chronic valvular damage.
The Imaging Cornerstone: Echocardiography's Pivotal Role
Echocardiography serves as the definitive imaging tool for diagnosing and managing rheumatic heart disease (RHD). Its critical value can be understood through several key aspects:
- Superior Diagnostic Sensitivity: It can detect subtle valvular abnormalities missed by auscultation, enabling diagnosis of subclinical RHD where no audible murmur is present.
- Standardized Diagnostic Criteria: The World Heart Federation (WHF) evidence-based criteria provide a unified framework for classifying "borderline" and "definite" RHD based on specific morphological and Doppler findings, ensuring diagnostic consistency.
- Dual-Phase Application: Echocardiography is indispensable in both the acute phase, to confirm and quantify carditis during acute rheumatic fever (ARF), and the chronic phase, for monitoring valvular damage progression and guiding long-term management.
- Revolutionizing Screening: The portability of handheld devices has transformed public health efforts, making large-scale screening feasible in endemic, resource-limited regions and enabling early intervention.
The Laboratory's Critical Role: Confirming Infection and Inflammation
Laboratory testing provides the essential, objective evidence required to support the clinical diagnosis of acute rheumatic fever (ARF) and rheumatic heart disease (RHD). Its role is twofold: to confirm a preceding group A streptococcal (GAS) infection and to document the associated systemic inflammatory response.
Confirming Preceding Streptococcal Infection
Serological testing is essential to provide objective proof of a recent group A streptococcal infection, a mandatory requirement for diagnosing Acute Rheumatic Fever. The core biomarkers are the antistreptolysin O (ASO) titer and anti-DNase B titer, with elevated levels confirming prior exposure and supporting the immune-mediated pathogenesis of the disease.
Documenting Systemic Inflammation
Measuring acute-phase reactants is crucial for documenting the systemic inflammatory response characteristic of acute rheumatic fever. Elevated levels of C-reactive protein (CRP) and an increased erythrocyte sedimentation rate (ESR) serve as key minor criteria in the Jones criteria, providing laboratory evidence of active inflammation and supporting the clinical diagnosis.
The Future is Now: The Quest for Novel Biomarkers
hile current diagnostics rely on established serological and inflammatory markers, a significant unmet need remains for specific biomarkers capable of precisely diagnosing acute rheumatic fever (ARF), stratifying risk for rheumatic heart disease (RHD) progression, and monitoring disease activity. The quest for novel biomarkers aims to move beyond merely confirming a past streptococcal infection or non-specific inflammation, towards identifying unique molecular signatures of the autoimmune pathology itself, which would enable earlier intervention and more personalized management.
- Inflammatory Cytokines: Markers such as IL-1β, IL-6, and TNF-α are being investigated to quantify the specific autoimmune-driven inflammatory cascade in ARF, potentially offering greater specificity than CRP or ESR.
- Autoantibodies: Research focuses on antibodies that mistakenly target host proteins in the heart (e.g., cardiac myosin, vimentin, laminin), which are believed to be direct mediators of valvular damage in RHD.
- Genetic Markers: Identifying genetic susceptibility loci (e.g., within the HLA complex) could help pinpoint individuals at highest risk for developing ARF following a streptococcal infection.
IVD Products for Rheumatic Heart Disease
As a specialized provider of in vitro diagnostic solutions, Alta DiagnoTech offers a comprehensive portfolio of innovative tests to support the accurate diagnosis and management of rheumatic heart disease (RHD). Our products are engineered to deliver reliable, timely results that enable healthcare providers to confirm preceding streptococcal infection, evaluate inflammatory activity, and facilitate research on novel biomarkers. If you have related needs, please feel free to contact us for more information or product support.
| Product Name |
Technology |
Application |
| Rapid Strep Antibody Test Kit (ASO) |
Immunochromatographic Lateral Flow Assay |
Qualitative detection of Anti-Streptolysin O antibodies for point-of-care screening of recent Group A Streptococcal infection. |
| High-Sensitivity Streptococcal Serology Assay Kit |
Chemiluminescent Immunoassay (CLIA) |
Quantitative measurement of ASO and Anti-DNase B antibody titers to provide laboratory-confirmed evidence of preceding streptococcal infection. |
| Automated Inflammation Panel (CRP/ESR) |
Immunoturbidimetry (CRP) / Automated ESR Analyzer |
Simultaneous assessment of C-Reactive Protein and Erythrocyte Sedimentation Rate to evaluate systemic inflammatory activity. |
| Cardiac Autoantibody Profiling Panel |
Multiplex Bead-Based Immunoassay |
Detection of autoantibodies against cardiac proteins (e.g., myosin, vimentin) for research and potential risk stratification. |
| Portable CRP Quantitative Test Kit |
Fluorescent Immunoassay Cartridge |
Point-of-care quantitative CRP testing for rapid assessment of inflammatory status in resource-limited settings. |
Reference
- Passos L S A, Nunes M C P, Aikawa E. Rheumatic heart valve disease pathophysiology and underlying mechanisms[J]. Frontiers in Cardiovascular Medicine, 2021, 7: 612716.
This article is for research use only. Do not use in any diagnostic or therapeutic application.



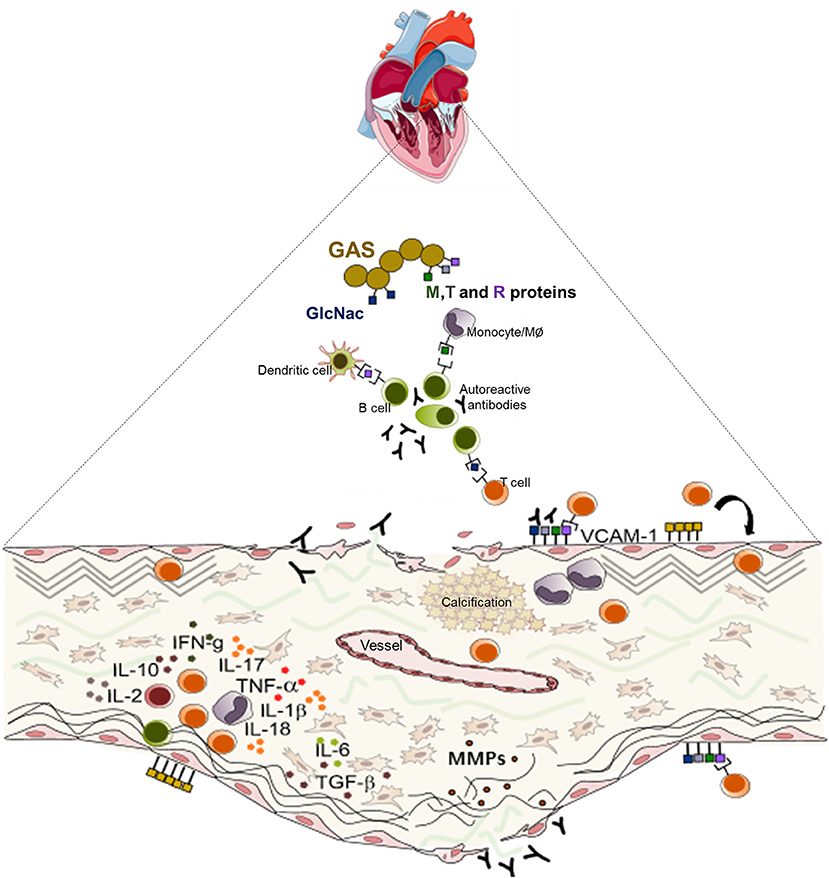 Fig.1 A schematic diagram illustrating the pathogenesis of rheumatic heart valve disease. (Passos L S A, et al., 2021)
Fig.1 A schematic diagram illustrating the pathogenesis of rheumatic heart valve disease. (Passos L S A, et al., 2021)