- Home
- Resource
- Disease Diagnosis
- Cardiovascular Diseases
- Diagnosing Dyslipidemia: A Guide to Lipid Profiling, Biomarkers, and Risk Assessment
- Home
- IVD
- By Technology Types
- By Diseases Types
- By Product Types
- Research
- Resource
- Distributors
- Company
Dyslipidemia is a common metabolic disorder characterized by imbalances in blood lipids that significantly increases the risk of cardiovascular diseases. This resource provides a comprehensive overview of the modern diagnostic approach for dyslipidemia, detailing the essential role of lipid profiling, advanced biomarkers, and integrated risk assessment in clinical practice.
Dyslipidemia is a metabolic disorder characterized by an imbalance in blood lipids, including elevated levels of low-density lipoprotein cholesterol (LDL-C) and triglycerides, along with low levels of high-density lipoprotein cholesterol (HDL-C). As a major modifiable risk factor for atherosclerotic cardiovascular disease (ASCVD), it contributes to the buildup of plaque in arteries, increasing the risk of heart attack and stroke. Often asymptomatic, its detection and management rely heavily on laboratory diagnostics, making accurate lipid profiling a cornerstone of preventive cardiovascular care.
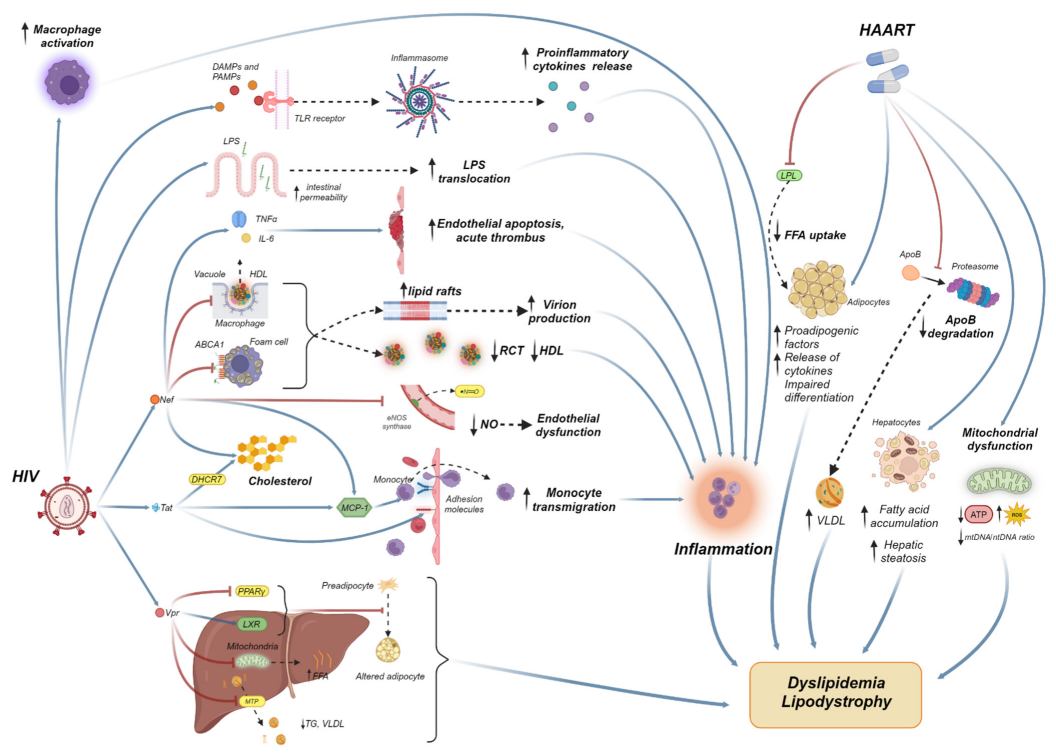 Fig.1 The pathogenesis of dyslipidemia in PLHIV under HAART. (Papantoniou E, et al., 2024)
Fig.1 The pathogenesis of dyslipidemia in PLHIV under HAART. (Papantoniou E, et al., 2024)
The standard lipid profile serves as the fundamental and first-line diagnostic tool in the identification and management of dyslipidemia. This panel of blood tests provides a quantitative snapshot of key lipids and lipoproteins in the circulation, offering critical insights into a patient's cardiovascular risk status. Its components are pivotal for initial screening, risk classification, and guiding therapeutic decisions. The core components of this profile are:

Low-Density Lipoprotein Cholesterol (LDL-C)
Often termed "bad cholesterol," LDL-C is the primary target for cholesterol-lowering therapy. It is the major carrier of cholesterol to peripheral tissues and is directly implicated in the formation of atherosclerotic plaque.
High-Density Lipoprotein Cholesterol (HDL-C)
Known as "good cholesterol," HDL-C facilitates the reverse transport of cholesterol from peripheral tissues back to the liver for excretion. Low levels are independently associated with increased cardiovascular risk.
Triglycerides (TG)
These are the most common type of fat in the body, originating from dietary intake and liver production. Elevated levels are a significant marker of cardiovascular risk and can contribute to pancreatitis at very high concentrations.

Total Cholesterol
This measures the total amount of cholesterol carried in all lipoprotein particles (including LDL, HDL, and VLDL). While a useful overall marker, it must be interpreted in the context of its sub-fractions.
Interpreting a lipid profile extends far beyond simply comparing numbers to a reference range. The clinical significance of any given result is profoundly influenced by the individual's overall cardiovascular risk profile. A borderline-elevated LDL-C level, for instance, represents a substantially greater threat to a patient with additional risk factors than to one without. Therefore, accurate diagnosis and management planning require integrating lipid data with a comprehensive risk assessment.

This integrative approach utilizes validated risk prediction algorithms, such as the Pooled Cohort Equations (PSC), which estimate a patient's 10-year risk for Atherosclerotic Cardiovascular Disease (ASCVD). These tools synthesize information including age, sex, blood pressure, cholesterol levels, diabetes status, and smoking history to generate a personalized risk score. The outcome of this assessment is what ultimately guides the clinical response—determining the intensity of lifestyle counseling, the necessity of pharmacologic therapy, and the appropriate aggressiveness of LDL-C treatment targets. This strategy ensures that patient care is not based on isolated lab values, but on a holistic understanding of their individual risk for future cardiovascular events.
While the standard lipid profile is the essential starting point, a significant portion of cardiovascular risk remains unexplained by LDL-C, HDL-C, and triglycerides alone. This residual risk often necessitates a deeper dive into the lipidome using advanced biomarkers that provide a more precise and comprehensive assessment of atherogenic burden. These markers are critical for refining risk stratification in complex cases, such as patients with familial hypercholesterolemia, metabolic syndrome, or a strong personal or family history of ASCVD despite seemingly acceptable standard lipid levels.

Apolipoprotein B (ApoB) is a structural protein found on all atherogenic lipoproteins, including LDL, VLDL, and their remnants. Since each of these harmful particles contains a single ApoB molecule, measuring ApoB provides a direct count of the total number of atherogenic particles in the blood. This makes it a more accurate indicator of cardiovascular risk than LDL-C, especially in individuals with obesity, diabetes, or metabolic syndrome where cholesterol content per particle can vary.

Lipoprotein(a) (Lp(a)) is a unique, genetically determined particle that consists of an LDL-like molecule bound to a specific protein called apolipoprotein(a). Elevated Lp(a) is an independent, causal, and common risk factor for atherosclerotic cardiovascular disease and aortic stenosis. Its levels are largely unaffected by lifestyle, making it a crucial marker for identifying inherited risk, and typically requires a one-time measurement to guide lifelong risk assessment.

Non-HDL-C is a simple but powerful calculated parameter representing the total cholesterol content within all atherogenic lipoproteins. It is derived by subtracting HDL-C from total cholesterol, thereby capturing the cholesterol in LDL, VLDL, IDL, and Lp(a). Non-HDL-C is increasingly recognized as a superior secondary treatment target after LDL-C, as it provides a comprehensive estimate of atherogenic burden without the need for a fasting sample.

Other notable markers such as apolipoprotein A-I (Apo A-I), the main protein component of HDL, and HDL particle number (HDL-P), offer a more nuanced view of the protective, reverse cholesterol transport pathway. These markers can help further refine risk assessment, particularly in patients with discordant HDL-C levels, providing insight into the quality and functionality of HDL particles beyond their cholesterol content.
As a leader in cardiovascular disease diagnostics, Alta DiagnoTech offers a comprehensive portfolio of high-precision solutions for dyslipidemia testing. Our product range covers the complete diagnostic spectrum, from routine lipid profiling to advanced biomarker analysis, enabling accurate cardiovascular risk assessment and stratification through reliable assay performance. If you have related needs, please feel free to contact us for more information or product support.
| Product Name | Technology | Application |
| Direct LDL-C Assay Kit | Enzymatic Colorimetric Method | Quantitative measurement of low-density lipoprotein cholesterol in human serum/plasma |
| Lipoprotein(a) [Lp(a)] Assay | Latex-Enhanced Immunoturbidimetry | Quantitative determination of Lp(a) for cardiovascular risk assessment |
| Apolipoprotein B (ApoB) Assay | Immunoturbidimetric Assay | Quantitative measurement of apolipoprotein B in human serum/plasma |
| HDL-C Direct Assay Kit | Homogeneous Enzymatic Colorimetric Assay | Direct quantitative measurement of high-density lipoprotein cholesterol |
| Apolipoprotein A-I Assay | Immunonephelometry | Quantitative determination of apolipoprotein A-I in human serum |
| Triglycerides Assay Kit | Enzymatic Colorimetric Method | Quantitative measurement of triglycerides in human serum/plasma |
Reference
This article is for research use only. Do not use in any diagnostic or therapeutic application.
|
There is no product in your cart. |