Antiphospholipid syndrome (APS) is an autoimmune disorder characterized by blood clots and pregnancy complications, diagnosed through the integration of specific clinical events and persistent laboratory findings. This resource decodes the APS diagnostic journey, providing a clear guide from recognizing clinical suspicion, through comprehensive antibody profiling, to the critical steps of confirmatory testing and differential diagnosis required for an accurate and definitive diagnosis.
Overview of Antiphospholipid Syndrome (APS)
Antiphospholipid syndrome (APS) is a systemic autoimmune disorder characterized by the persistent presence of antiphospholipid antibodies in the blood, which leads to an increased risk of vascular thrombosis (both arterial and venous) and/or pregnancy-related complications such as recurrent miscarriage, fetal death, or severe preeclampsia. Diagnosis follows strict international criteria (Sydney criteria), requiring the combination of at least one clinical event (thrombosis or pregnancy morbidity) and laboratory confirmation of one or more specific antibodies—lupus anticoagulant, anti-cardiolipin antibodies, or anti-β2-glycoprotein I antibodies—on two or more occasions at least 12 weeks apart.
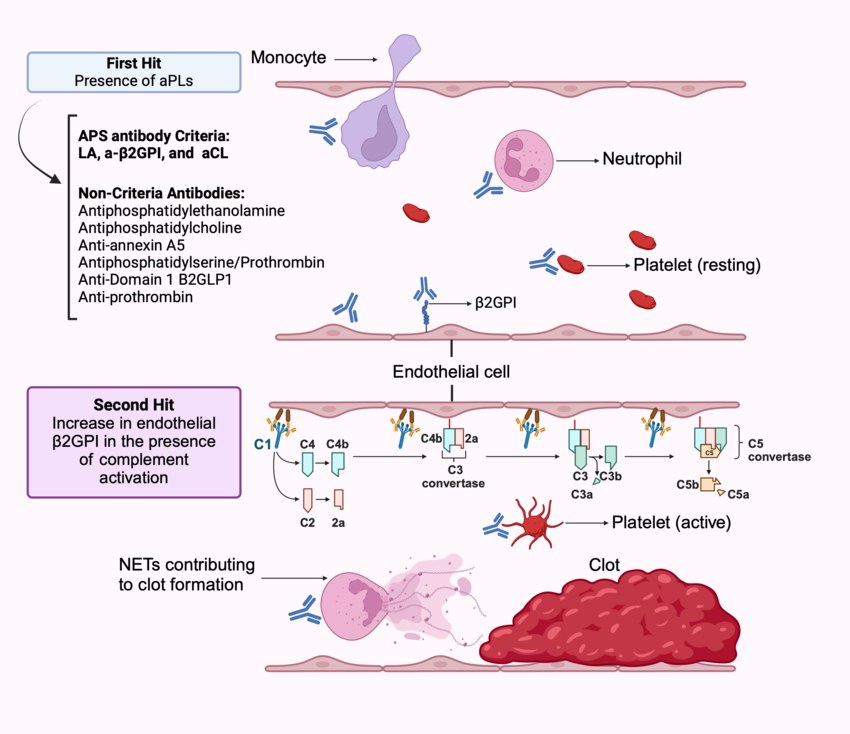 Fig.1 Pathophysiology of antiphospholipid syndrome (APS). (Kortright-Maldonado, Karen, et al., 2025)
Fig.1 Pathophysiology of antiphospholipid syndrome (APS). (Kortright-Maldonado, Karen, et al., 2025)
Clinical Suspicion of Antiphospholipid Syndrome (APS)
Clinical suspicion for antiphospholipid syndrome (APS) should be strongly considered in any patient presenting with an unexplained venous, arterial, or small-vessel thrombosis, especially at a young age (<50 years) or in an unusual anatomic location (e.g., cerebral, mesenteric). It is also a key diagnostic consideration in individuals with a history of specific, severe pregnancy complications, such as recurrent early miscarriages, unexplained fetal death after 10 weeks, or premature birth due to severe preeclampsia or placental insufficiency. This suspicion is further heightened in patients with other autoimmune conditions, particularly systemic lupus erythematosus (SLE), or those with a known family history of APS or thrombosis.
Antibody Profiling of Antiphospholipid Syndrome (APS)
Laboratory confirmation of antiphospholipid syndrome (APS) hinges on the detection of a specific set of autoantibodies, collectively known as antiphospholipid antibodies. Profiling for these three core biomarkers is essential, as diagnosis requires at least one to be persistently positive, and the presence of multiple antibodies ("triple positivity") signifies the highest risk for thrombotic events.
Lupus Anticoagulant (LA)
Lupus anticoagulant (LA) is not a single antibody but a functional phenomenon detected by phospholipid-dependent coagulation assays that paradoxically prolong clotting times in vitro. Its identification requires a multi-step testing algorithm (e.g., using DRVVT and APTT-based methods) to confirm the presence of an inhibitor and rule out other causes of prolonged clotting. It is one of the most specific laboratory criteria for APS.
Anti-Cardiolipin Antibodies (aCL)
Anti-cardiolipin antibodies (aCL) are directed against cardiolipin, a phospholipid component of cell membranes. They are detected via solid-phase immunoassays (like ELISA) and must be present at medium or high titers (typically >40 GPL or MPL units) for diagnostic significance according to classification criteria. Testing includes both IgG and IgM isotypes, with IgG isotype being more strongly associated with clinical events.
Anti-β2-Glycoprotein I Antibodies (anti-β2GPI)
Anti-β2-glycoprotein I antibodies (anti-β2GPI) target a plasma protein that binds to phospholipids. Also detected by immunoassay, these antibodies are considered highly specific for APS. Similar to aCL, only IgG and/or IgM isotypes at medium/high titers are considered diagnostically relevant. The presence of anti-β2GPI antibodies, especially IgG, carries a strong association with thrombosis and pregnancy morbidity.
Confirmatory Testing and Exclusion of Antiphospholipid Syndrome (APS)
A positive antiphospholipid antibody test alone is not sufficient for diagnosis; definitive confirmation of antiphospholipid syndrome (APS) requires adherence to strict laboratory protocols and the systematic exclusion of alternative causes. This phase ensures that detected antibodies are persistently abnormal and specifically linked to APS, rather than a temporary or secondary finding.
The 12-Week Rule
The 12-week rule is a mandatory diagnostic criterion requiring that any positive antiphospholipid antibody test (for lupus anticoagulant, anti-cardiolipin, or anti-β2-glycoprotein I) must be persistently positive on a second sample drawn at least 12 weeks after the first. This rule is crucial for distinguishing persistent, clinically significant autoimmunity from transient antibody positivity that can occur due to infections, certain medications, or other acute illnesses.
Differential Diagnosis and Exclusion
Differential diagnosis and exclusion involve actively ruling out other potential causes of thrombosis or pregnancy loss before confirming APS. This includes testing for inherited thrombophilias (e.g., Factor V Leiden), evaluating for malignancy, assessing for other autoimmune diseases (notably Systemic Lupus Erythematosus, which can occur concurrently with APS), and investigating other causes of recurrent miscarriage or vascular events.
Applying the Sydney Classification Criteria in Practice
The practical application of the Sydney classification criteria for antiphospholipid syndrome (APS) involves a systematic, two-part assessment where both a qualifying clinical event and persistent laboratory evidence must be met.
- First, it must be confirmed that the patient has experienced at least one defined clinical criterion, such as objectively verified vascular thrombosis or specific pregnancy morbidity.
- Second, laboratory testing must demonstrate the persistent presence (confirmed≥12 weeks apart) of at least one of the three core antiphospholipid antibodies: lupus anticoagulant, anti-cardiolipin antibodies (IgG/IgM at medium/high titer), or anti-β2-glycoprotein I antibodies (IgG/IgM at medium/high titer).
A diagnosis is established only when both domains are conclusively satisfied, excluding other causes.
IVD Products for Antiphospholipid Syndrome (APS)
To meet the stringent and complex diagnostic requirements of antiphospholipid syndrome (APS), Alta DiagnoTech provides a comprehensive portfolio of in vitro diagnostic (IVD) solutions. Our integrated assays and automated systems are designed to support the complete diagnostic algorithm, delivering the precise and reliable results needed for accurate classification and clinical decision-making. If you have related needs, please feel free to contact us for more information or product support.
| Product Name |
Technology |
Application |
| Lupus Anticoagulant (LA) Screening & Confirmatory Kit |
Coagulation Assay (e.g., Dilute Russell's Viper Venom Time - dRVVT, Activated Partial Thromboplastin Time - aPTT) |
Integrated multi-step testing system for the detection and confirmation of Lupus Anticoagulant activity in platelet-poor plasma, following international guideline algorithms. |
| Anti-Cardiolipin (aCL) Antibody ELISA Kit (IgG/IgM) |
Enzyme-Linked Immunosorbent Assay (ELISA) |
Quantitative measurement of IgG and/or IgM anti-Cardiolipin antibodies in human serum or plasma, essential for APS laboratory criteria with defined medium/high titer thresholds. |
| Anti-β2-Glycoprotein I (anti-β2GPI) Antibody ELISA Kit (IgG/IgM) |
Enzyme-Linked Immunosorbent Assay (ELISA) |
Quantitative measurement of IgG and/or IgM anti-β2-Glycoprotein I antibodies in human serum or plasma, a highly specific test for APS diagnosis. |
| Automated Coagulation Analyzer with LA Testing Package |
Automated Photometric Coagulation Analysis |
A high-throughput, automated platform for performing LA testing algorithms (screening, mixing, confirmatory steps) with standardized reagents and precise result calculation, ensuring workflow efficiency and consistency. |
| Autoimmune Coagulopathy Panel (APC Resistance, Protein C/S, etc.) |
Coagulation & Chromogenic Assays |
A comprehensive testing panel to rule out inherited thrombophilias and other acquired coagulopathies, supporting the differential diagnosis required before confirming APS. |
Reference
- Kortright-Maldonado, Karen, et al. "Navigating antiphospholipid syndrome: from personalized therapies to cutting-edge research." Rheumatology Advances in Practice 9.1 (2025): rkaf005.
This article is for research use only. Do not use in any diagnostic or therapeutic application.



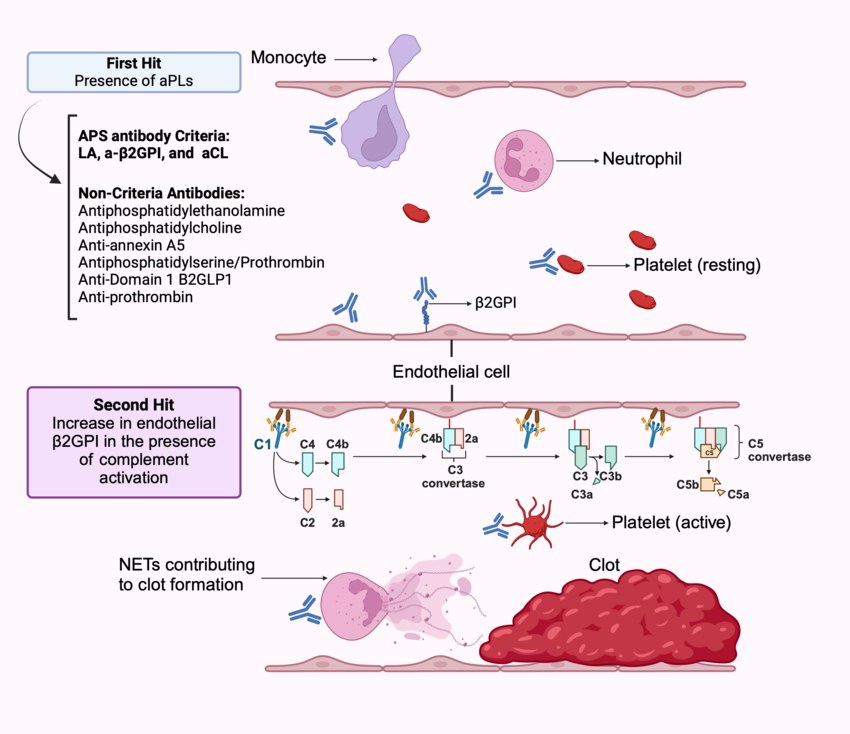 Fig.1 Pathophysiology of antiphospholipid syndrome (APS). (Kortright-Maldonado, Karen, et al., 2025)
Fig.1 Pathophysiology of antiphospholipid syndrome (APS). (Kortright-Maldonado, Karen, et al., 2025)