Pulmonary embolism (PE) and deep vein thrombosis (DVT) represent critical cardiovascular emergencies where timely and accurate diagnosis is paramount. This resource provides a comprehensive guide to the modern diagnostic approach for venous thromboembolism (VTE), detailing how cardiovascular biomarkers are integrated into clinical pathways to optimize patient triage, risk stratification, and ultimately improve outcomes.
Overview of Pulmonary Embolism (PE) & Deep Vein Thrombosis (DVT)
Pulmonary embolism (PE) and deep vein thrombosis (DVT) are two clinical manifestations of venous thromboembolism (VTE), a serious cardiovascular condition characterized by abnormal blood clot formation. DVT typically occurs when a thrombus forms in the deep veins of the legs or pelvis, while PE represents the potentially life-threatening complication that arises when such a clot dislodges and travels to the pulmonary arteries, obstructing blood flow to the lungs. This condition constitutes a medical emergency, and its diagnosis relies heavily on a combination of clinical assessment, biomarker testing and confirmatory imaging studies to enable rapid intervention and prevent fatal outcomes.
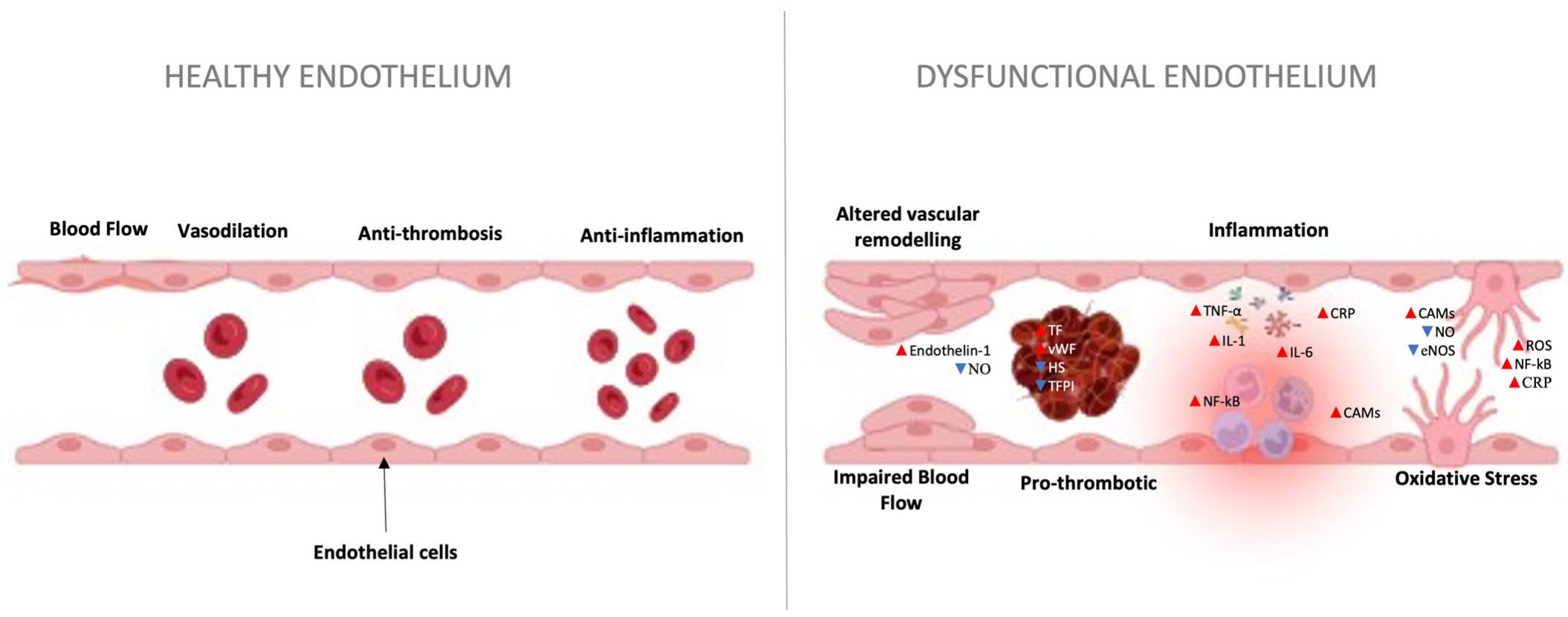 Fig.1 Effects of pulmonary embolism (PE) in the vascular endothelium. (Peracaula M, et al., 2024)
Fig.1 Effects of pulmonary embolism (PE) in the vascular endothelium. (Peracaula M, et al., 2024)
Cornerstone Biomarker for PE & DVT Diagnostics
D-dimer is a specific protein fragment, or fibrin degradation product, that is generated when a blood clot in the body undergoes breakdown through the natural process of fibrinolysis. Its presence in the blood signifies that significant coagulation and subsequent clot dissolution have occurred, making it a direct biological marker of thrombotic activity. Its main clinical applications include:
- Primary Rule-Out Tool for VTE: Its foremost application is the exclusion of Venous Thromboembolism (VTE). A negative D-dimer test result, in conjunction with a low clinical pre-test probability, can reliably rule out acute PE or DVT with a very high degree of safety, thereby avoiding unnecessary imaging tests.
- Triage in Suspected DVT: For patients with suspected Deep Vein Thrombosis, a negative D-dimer test effectively excludes the diagnosis in outpatient settings with low to moderate clinical probability, guiding further management decisions.
- Exclusion of Pulmonary Embolism: In the emergency department, it is the primary biomarker used to rule out PE in patients assessed as having a low or intermediate pre-test probability, significantly streamlining the diagnostic pathway.
- Aid in Diagnosing Other Conditions: While less specific, elevated D-dimer levels can also support the diagnosis of other thrombotic conditions, such as disseminated intravascular coagulation (DIC).
Cardiac Biomarkers for Risk Stratification in PE
While D-dimer serves as an essential tool for the initial exclusion of pulmonary embolism, its utility diminishes once the diagnosis is confirmed. At this critical juncture, the clinical focus shifts from detection to risk stratification, where cardiac biomarkers provide vital prognostic information to guide management strategies. These biomarkers objectively quantify the degree of right ventricular dysfunction caused by the acute pressure overload, enabling clinicians to identify patients at high risk for adverse outcomes and tailor treatment intensity accordingly. Key biomarkers include:
Cardiac Troponin (cTn/I or hs-cTn)
This biomarker is a highly specific indicator of myocardial injury. In acute PE, the sudden pressure overload on the right ventricle can lead to ischemia and micro-infarction of the right ventricular wall. Elevated troponin levels, therefore, directly reflect this cardiomyocyte damage and are a powerful predictor of increased short-term mortality and complications, such as cardiogenic shock.
B-type Natriuretic Peptide (BNP) / NT-proBNP
These peptides are released primarily from the cardiac ventricles in response to myocardial stretch and increased wall tension. In the context of acute PE, elevated levels of BNP or NT-proBNP are a sensitive marker of right ventricular dysfunction and dilatation. Their elevation signals a failure of the right ventricle to adapt to the afterload stress and is strongly associated with clinical deterioration and poor prognosis.
The Integrated Diagnostic Pathway: Putting Biomarkers to Work
The modern diagnostic approach for venous thromboembolism (VTE) is not a linear process but a strategic, sequential pathway that intelligently integrates clinical assessment with biomarker testing and imaging to maximize both efficiency and patient safety. This algorithm is designed to rapidly rule out the disease in low-risk patients while ensuring high-risk cases receive prompt, definitive confirmation. Biomarkers, particularly D-dimer, serve as the crucial decision points in this pathway, guiding clinicians on when to safely stop further testing or when to proceed to more complex imaging. The core steps of this biomarker-driven pathway are:
- Initial Clinical Probability Assessment: The diagnostic pathway is initiated by applying a validated clinical prediction rule, such as the wells score or revised geneva score, to stratify patients into low, intermediate, or high pre-test probability categories. This critical first step determines the entire subsequent diagnostic sequence, ensuring an efficient and risk-appropriate approach.
- Biomarker Triage and Rule-Out: For patients categorized as low or intermediate probability, a quantitative D-dimer test serves as a pivotal triage tool. A negative result reliably excludes venous thromboembolism (VTE), effectively concluding the diagnostic workup, while a positive result necessitates progression to definitive imaging studies.
- Definitive Imaging for Confirmation: Confirmatory imaging is indicated following a positive D-dimer test or in high-probability cases. Computed tomography pulmonary angiography (CTPA) provides definitive diagnosis for suspected pulmonary embolism, while compression ultrasonography (CUS) serves as the gold standard for confirming deep vein thrombosis.
- Post-Diagnosis Risk Stratification: Following PE confirmation, cardiac biomarkers including cardiac troponin and BNP/NT-proBNP are utilized for risk stratification. Elevated levels of these biomarkers indicate right ventricular dysfunction, identifying high-risk patients who may require intensified monitoring and advanced therapeutic interventions.
Featured Products for PE & DVT Diagnostics
As a leader in cardiovascular disease diagnostics, Alta DiagnoTech provides a comprehensive portfolio of high-performance IVD solutions for pulmonary embolism (PE) and deep vein thrombosis (DVT). Our robust assays deliver critical diagnostic and prognostic data across the entire clinical workflow—from initial VTE exclusion using D-dimer to advanced risk stratification with cardiac biomarkers—empowering clinicians to make confident, timely decisions for improved patient outcomes. If you have related needs, please feel free to contact us for more information or product support.
| Product Name |
Technology |
Application |
| D-dimer Assay |
Immunoturbidimetric Latex Assay |
Quantitative measurement for exclusion of venous thromboembolism (VTE) in low/moderate risk patients. |
| High-Sensitivity Troponin I Assay |
Chemiluminescent Immunoassay (CLIA) |
Precise detection of myocardial injury for risk stratification in confirmed pulmonary embolism. |
| NT-proBNP Assay |
Chemiluminescent Immunoassay (CLIA) |
Quantitative measurement for assessment of right ventricular dysfunction in acute PE. |
| Fibrinogen Assay |
Clotting Method |
Functional measurement of fibrinogen levels in coagulation assessment. |
| Anti-Xa Assay |
Chromogenic Method |
Monitoring heparin anticoagulant therapy effectiveness. |
Reference
- Peracaula M, Sebastian L, Francisco I, et al. Decoding pulmonary embolism: Pathophysiology, diagnosis, and treatment[J]. Biomedicines, 2024, 12(9): 1936.
This article is for research use only. Do not use in any diagnostic or therapeutic application.



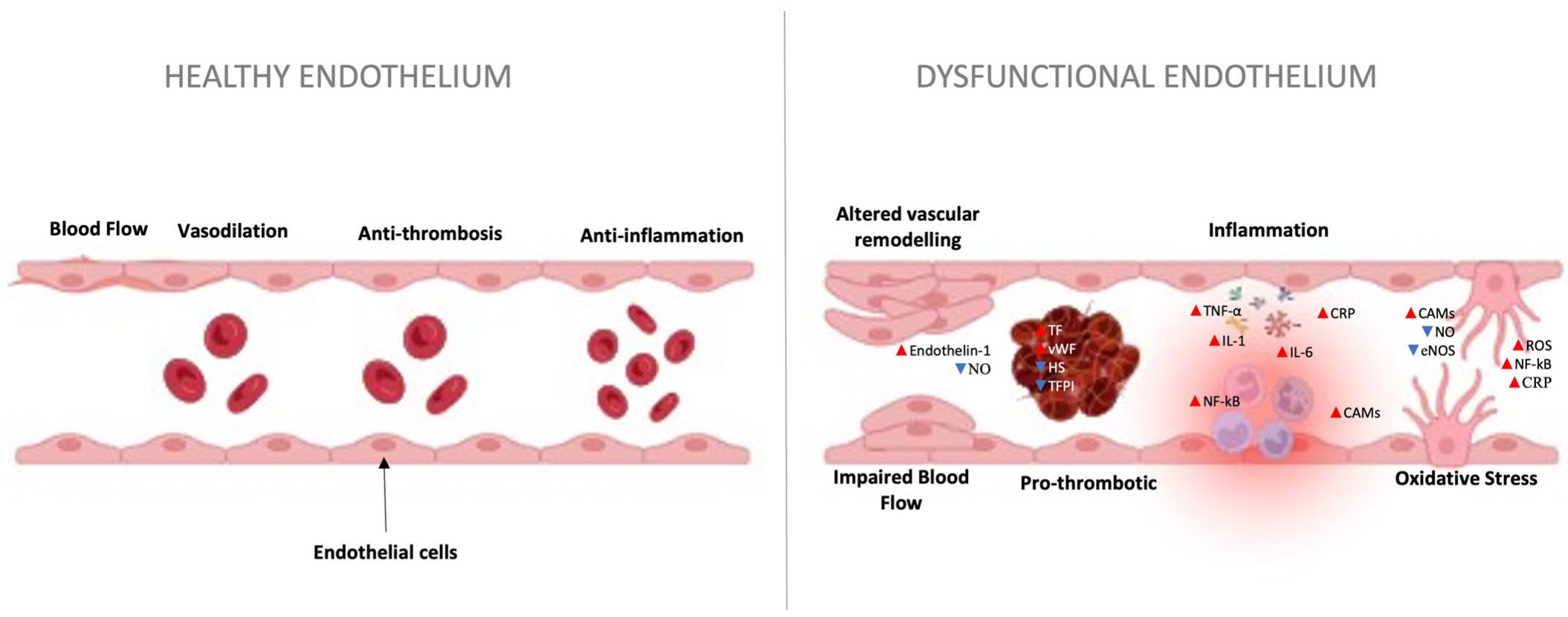 Fig.1 Effects of pulmonary embolism (PE) in the vascular endothelium. (Peracaula M, et al., 2024)
Fig.1 Effects of pulmonary embolism (PE) in the vascular endothelium. (Peracaula M, et al., 2024)

