- Home
- Resource
- Disease Diagnosis
- Endocrine Diseases
- Biomarkers of Hyperthyroidism: From TSH Suppression to Autoimmune Confirmation
- Home
- IVD
- By Technology Types
- By Diseases Types
- By Product Types
- Research
- Resource
- Distributors
- Company
Hyperthyroidism is a metabolic disorder characterized by excessive thyroid hormone production, leading to a wide range of symptoms from palpitations to weight loss. This resource provides a comprehensive guide to the essential biomarkers and diagnostic pathway for hyperthyroidism, detailing the critical roles of TSH suppression, thyroid hormone (T4/T3) elevation, and TRAb testing in confirming diagnosis, assessing severity, and determining the underlying autoimmune cause.
Hyperthyroidism is a metabolic disorder characterized by the overproduction of thyroid hormones from the thyroid gland, leading to accelerated body metabolism. This condition manifests through symptoms such as unintentional weight loss, rapid heartbeat, heat intolerance, tremors, and anxiety. The most common cause is Graves' disease, an autoimmune disorder where antibodies stimulate the thyroid to produce excess hormones, though other causes include toxic nodules and thyroiditis. Diagnosis relies heavily on laboratory testing demonstrating suppressed TSH with elevated thyroid hormone levels (T4 and T3), complemented by antibody testing to determine the underlying etiology, with treatment strategies varying from anti-thyroid medications to radioactive ablation based on the specific cause and severity.
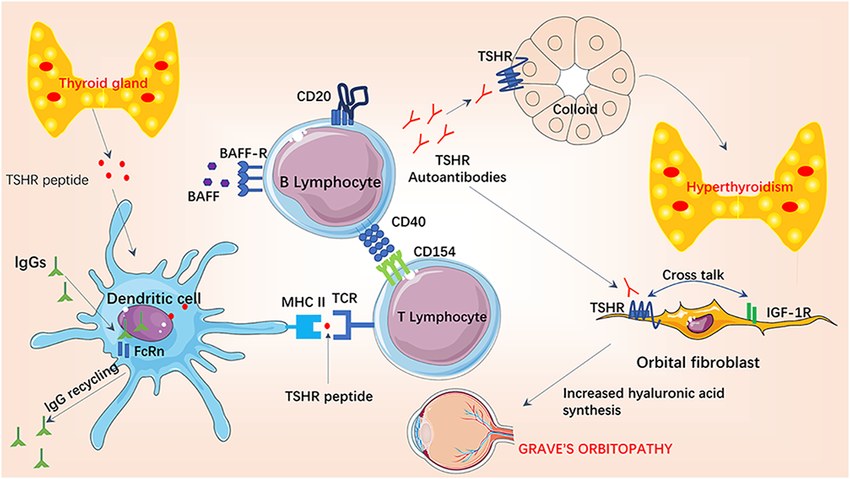 Fig.1 Pathogenesis of Graves' hyperthyroidism and Graves’ orbitopathy. (He Q, et al., 2022)
Fig.1 Pathogenesis of Graves' hyperthyroidism and Graves’ orbitopathy. (He Q, et al., 2022)

Thyroid-stimulating hormone (TSH) serves as the cornerstone and most sensitive initial test in the diagnosis of hyperthyroidism, functioning as the primary indicator of thyroid-pituitary axis disruption. In hyperthyroid states, elevated levels of circulating thyroid hormones (T4 and T3) suppress pituitary TSH production through negative feedback, resulting in characteristically low or undetectable TSH levels. This suppression makes TSH an excellent screening tool, as it typically becomes abnormal before thyroid hormone levels rise beyond reference ranges in developing hyperthyroidism. However, while a suppressed TSH reliably indicates probable thyrotoxicosis, it cannot determine the underlying etiology, necessitating further testing with thyroid hormones (free T4 and T3) and additional biomarkers to confirm the diagnosis and identify the specific cause.
The biochemical confirmation of hyperthyroidism relies fundamentally on the measurement of circulating thyroid hormones—free thyroxine (FT4) and triiodothyronine (T3). While a suppressed TSH indicates pituitary feedback, it is the elevated levels of FT4 and/or T3 that directly confirm the state of thyrotoxicosis and help characterize its severity and pattern. Understanding their distinct roles is essential for accurate diagnosis and differentiation between various forms of hyperthyroidism.

Pathophysiology
FT4 is the primary hormone secreted by the thyroid gland, with most circulating T3 derived from its peripheral conversion. In hyperthyroidism, thyroid overproduction leads to elevated levels of one or both hormones. The measurement of FT4 assesses the gland's direct secretory output, while T3 reflects both secretion and peripheral conversion. In conditions like Graves' disease, T3 elevation can be disproportionate to T4 (T3-toxicosis), a key pathophysiological hallmark.

Diagnostic Utility
FT4 is the cornerstone for confirming thyrotoxicosis when elevated in conjunction with a suppressed TSH. T3 measurement is critical for detecting cases where FT4 is normal but T3 is elevated—a scenario known as T3 toxicosis, which is common in early or recurrent Graves' disease and toxic nodules. The FT4/T3 ratio can provide clues to the underlying etiology, with Graves' disease often showing a higher T3 predominance compared to thyroiditis.

Clinical Applications
In practice, concurrent measurement of FT4 and T3 is recommended when hyperthyroidism is strongly suspected. This combined approach ensures the detection of T3-predominant disease, provides biochemical severity assessment to guide treatment urgency, and aids in etiological differentiation. Furthermore, T3 levels are particularly valuable for monitoring treatment response in Graves' disease, where T3 normalization may lag behind FT4.
TSH receptor antibody (TRAb) testing is a critical serological tool used to definitively determine the autoimmune etiology of hyperthyroidism, specifically for Graves' disease. Unlike tests that confirm the presence of thyrotoxicosis, TRAb testing identifies the underlying cause by detecting pathogenic antibodies that bind to and stimulate the thyroid-stimulating hormone (TSH) receptor. This leads to unregulated overproduction of thyroid hormones (T4 and T3) and is the key pathological mechanism in over 70% of hyperthyroidism cases. Key aspects of TRAb testing include:

TRAbs are autoantibodies that mimic the action of TSH. By continuously activating the TSH receptor on thyroid follicular cells, they cause uncontrolled thyroid hormone synthesis and secretion, thyroid growth (goiter), and in some cases, inflammation of the orbital tissues (thyroid eye disease).

A positive TRAb test is highly specific for Graves' disease. In the correct clinical context, it can be considered a definitive diagnostic finding, often eliminating the need for a radioactive iodine uptake (RAIU) scan to confirm the etiology. It is particularly valuable in atypical presentations and for confirming the diagnosis in pregnancy, where RAIU is contraindicated.

Beyond initial diagnosis, TRAb testing has prognostic value. High TRAb levels in a pregnant individual with Graves' disease are associated with an increased risk of fetal and neonatal thyroid dysfunction due to the transplacental passage of these stimulating antibodies. Furthermore, monitoring TRAb levels can help guide the duration of antithyroid drug therapy and assess the risk of relapse after medication withdrawal.
Specializing in precision diagnostics for endocrine disorders, Alta DiagnoTech provides a comprehensive portfolio of advanced in vitro diagnostic (IVD) solutions to support the complete diagnostic workflow for hyperthyroidism. Our robust testing menu enables clinicians to accurately confirm thyrotoxicosis, determine disease severity, and identify the underlying etiology through fully automated and highly specific immunoassays. If you have related needs, please feel free to contact us for more information or product support.
| Product Name | Technology | Application |
| High-Sensitivity TSH Assay Kit | Chemiluminescent Immunoassay (CLIA) | Initial screening and detection of TSH suppression in suspected hyperthyroidism |
| Free T4/T3 Quantitative Assay Panel | Chemiluminescent Immunoassay (CLIA) | Confirmation of thyrotoxicosis and assessment of biochemical severity |
| TRAb (TSH Receptor Antibody) Detection Kit | Automated Immunoassay | Definitive diagnosis of Graves' disease and differential diagnosis |
| Thyroid Autoantibody Panel (TPO/Tg) | Chemiluminescent Immunoassay (CLIA) | Supporting evidence for autoimmune thyroid disease |
| Thyroid Function Comprehensive Testing Panel | Automated Immunoassay System | Simultaneous evaluation of TSH, FT4, and T3 for complete assessment |
Reference
This article is for research use only. Do not use in any diagnostic or therapeutic application.
|
There is no product in your cart. |