- Home
- Resource
- Disease Diagnosis
- Endocrine Diseases
- Beyond Cortisol: The Integral Role of ACTH and Antibody Testing in Addison's Diagnosis
- Home
- IVD
- By Technology Types
- By Diseases Types
- By Product Types
- Research
- Resource
- Distributors
- Company
Addison's disease is a rare but serious endocrine disorder characterized by insufficient production of adrenal hormones, primarily cortisol and aldosterone. This resource provides a comprehensive guide to the diagnostic pathway for Addison's disease, detailing the essential laboratory tests including cortisol and ACTH measurements, ACTH stimulation testing, and autoantibody detection that enable clinicians to confirm adrenal insufficiency, determine its underlying cause, and guide appropriate treatment decisions.
Addison's disease, also known as primary adrenal insufficiency, is a rare but potentially life-threatening endocrine disorder characterized by the adrenal glands' inability to produce sufficient amounts of essential hormones, primarily cortisol and often aldosterone. This deficiency typically results from the autoimmune destruction of the adrenal cortex, though other causes include infections, genetic factors, or adrenal hemorrhage. The condition manifests through non-specific but progressive symptoms such as chronic fatigue, muscle weakness, weight loss, hyperpigmentation of the skin, and hypotension. Diagnosis relies heavily on laboratory confirmation of low cortisol levels, an inadequate response to ACTH stimulation testing, and frequently elevated ACTH levels, with treatment requiring lifelong hormone replacement therapy to manage the hormone deficiency and prevent adrenal crisis.
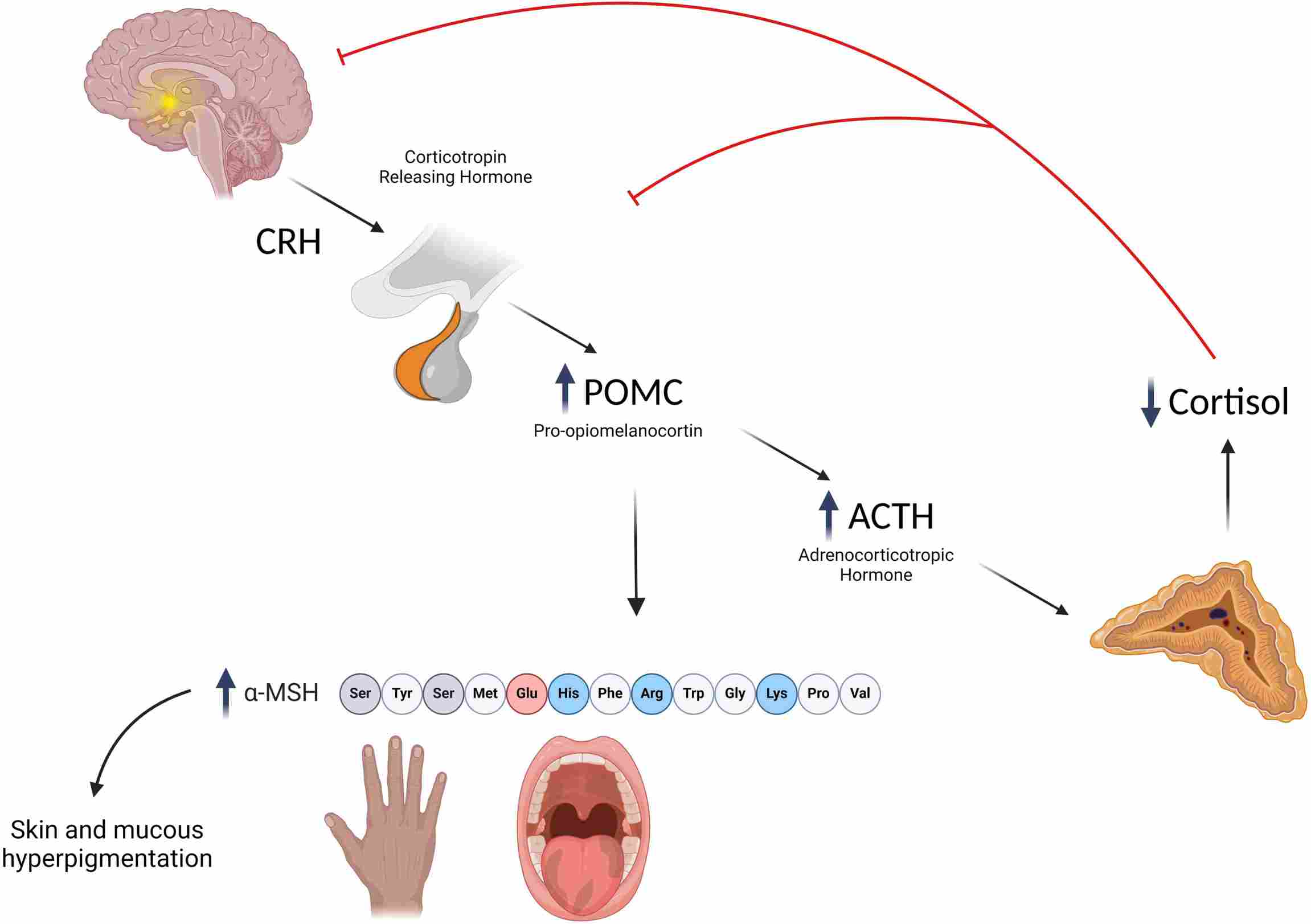 Fig.1 Mechanisms underlying the development of hyperpigmentation in primary adrenal insufficiency (Addison's disease). (Capalbo D, et al., 2024)
Fig.1 Mechanisms underlying the development of hyperpigmentation in primary adrenal insufficiency (Addison's disease). (Capalbo D, et al., 2024)

The definitive diagnosis of glucocorticoid deficiency is the cornerstone of confirming Addison's disease, requiring a systematic biochemical approach to demonstrate inadequate cortisol production. This process begins with a strong clinical suspicion based on symptoms like fatigue and hyperpigmentation, followed by laboratory confirmation through basal cortisol levels and, most critically, the ACTH stimulation test—the gold standard that reveals the adrenal glands' inability to mount an appropriate cortisol response. Accurate diagnosis at this stage is essential not only for initiating life-saving hormone replacement therapy but also for differentiating primary adrenal failure from other forms of adrenal insufficiency and guiding subsequent etiological investigation.
Adrenocorticotropic hormone (ACTH) measurement is essential for differentiating between primary and secondary adrenal insufficiency. In primary adrenal insufficiency (Addison's disease), the adrenal glands are damaged and cannot produce cortisol, leading to significantly elevated ACTH levels due to loss of negative feedback. In contrast, secondary adrenal insufficiency results from pituitary or hypothalamic dysfunction, causing low or inappropriately normal ACTH levels despite low cortisol.

Autoantibody testing plays a crucial role in determining the underlying etiology of Addison's disease, with approximately 80-90% of cases in developed countries being caused by autoimmune adrenalitis. The detection of specific autoantibodies provides definitive evidence of an autoimmune pathogenesis, helps distinguish autoimmune adrenal insufficiency from other causes (such as infections or genetic disorders), and prompts screening for other associated autoimmune conditions within the autoimmune polyglandular syndrome (APS) spectrum. Key autoantibody targets include:
21-Hydroxylase Antibodies (Anti-CYP21A2)
These are the primary and most specific serological markers for autoimmune Addison's disease, serving as a direct indicator of ongoing autoimmune attack against the adrenal cortex. Their presence strongly supports the diagnosis of autoimmune adrenalitis and may be detectable even before clinical symptoms manifest.

Other Associated Autoantibodies
In cases of autoimmune polyglandular syndrome, testing may be extended to include antibodies such as thyroid peroxidase (TPO) antibodies for Hashimoto's thyroiditis, glutamic acid decarboxylase (GAD) antibodies for type 1 diabetes, and intrinsic factor antibodies for pernicious anemia, providing a comprehensive assessment of coexisting autoimmune endocrinopathies.
Alta DiagnoTech offers a specialized portfolio of in vitro diagnostic (IVD) solutions to support the complete diagnostic evaluation of Addison's disease. Our comprehensive testing menu enables healthcare providers to accurately confirm adrenal insufficiency, differentiate its etiology, and identify associated autoimmune conditions through precise and reliable hormone and antibody assays. If you have related needs, please feel free to contact us for more information or product support.
| Product Name | Technology | Application |
| ACTH Stimulation Test Kit | Chemiluminescent Immunoassay (CLIA) | Gold-standard test for confirming primary adrenal insufficiency through cortisol response evaluation |
| Plasma ACTH Detection Kit | Chemiluminescent Immunoassay (CLIA) | Differential diagnosis between primary and secondary adrenal insufficiency |
| 21-Hydroxylase Antibody Assay | Enzyme-Linked Immunosorbent Assay (ELISA) | Specific detection of autoantibodies for confirming autoimmune adrenalitis |
| Adrenal Cortex Antibody Panel | Indirect Immunofluorescence (IIF) | Comprehensive detection of adrenal autoantibodies for autoimmune etiology investigation |
| Electrolyte and Renal Function Panel | Ion-Selective Electrode (ISE) & Photometric Assay | Assessment of characteristic electrolyte imbalances (hyponatremia, hyperkalemia) in Addison's disease |
| Autoimmune Polyglandular Syndrome Screening Panel | Multiplex Immunoassay | Simultaneous detection of multiple autoantibodies (thyroid, pancreatic, adrenal) for APS evaluation |
Reference
This article is for research use only. Do not use in any diagnostic or therapeutic application.
|
There is no product in your cart. |