Mycoplasma pneumoniae is a leading cause of community-acquired pneumonia in children, yet its diagnosis remains challenging due to atypical clinical presentations and limitations of conventional methods. This resource provides a comprehensive overview of modern diagnostic solutions, from clinical manifestations to cutting-edge detection technologies, empowering healthcare professionals to achieve accurate, timely diagnosis. Explore the following sections to understand key challenges and advanced strategies revolutionizing M. pneumoniae detection.
Introduction to Mycoplasma Pneumoniae Infection
Mycoplasma pneumoniae is a common but often underrecognized bacterial pathogen responsible for upper and lower respiratory tract infections, particularly in children and young adults. As a leading cause of community-acquired pneumonia (CAP), it presents atypically with persistent cough, mild fever, and wheezing, frequently mimicking viral illnesses. Unlike typical bacteria, M. pneumoniae lacks a cell wall, rendering it resistant to beta-lactam antibiotics and complicating treatment decisions.
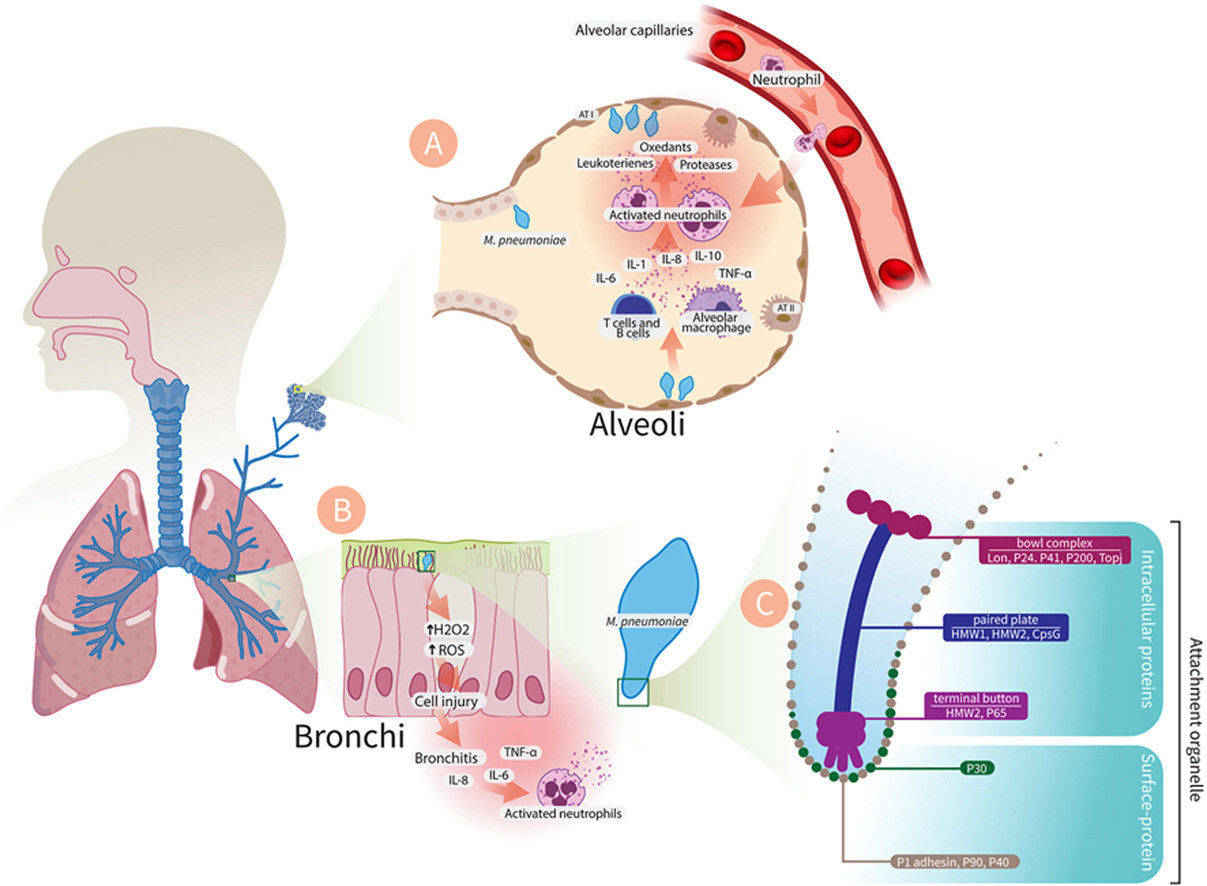 Fig.1 Pathogenesis of Mycoplasma pneumoniae infection. (Tahmasebi, Hamed, et al., 2024)
Fig.1 Pathogenesis of Mycoplasma pneumoniae infection. (Tahmasebi, Hamed, et al., 2024)
Clinical Manifestations of Mycoplasma Pneumoniae Infection in Children
M. pneumoniae infections in children exhibit a wide spectrum of clinical features, ranging from mild respiratory symptoms to severe extrapulmonary complications. Key manifestations include:
- Respiratory Symptoms:M. pneumoniae causes prolonged dry cough (3-4 weeks), mild fever, and wheezing. Pneumonia shows patchy infiltrates on X-ray despite mild exam findings. Upper respiratory symptoms (pharyngitis, nasal congestion) are common.
- Distinctive Features vs. Other Pneumonias:persistent cough with normal WBC, wheezing, and poor response to beta-lactams. Children often remain active ("walking pneumonia") despite radiographic pneumonia.
- Extrapulmonary Manifestations:May cause rashes (including Stevens-Johnson syndrome), hemolytic anemia, and neurologic complications (encephalitis, Guillain-Barré). These typically appear 1-3 weeks after respiratory symptoms.
Modern Diagnostic Solutions for Mycoplasma Pneumoniae Infection
Accurate diagnosis of Mycoplasma pneumoniae infection remains challenging due to its atypical clinical presentation and limitations of conventional methods. Modern diagnostic approaches have evolved to overcome these hurdles, offering improved sensitivity, specificity, and turnaround time.
Molecular Testing
PCR-based methods represent the gold standard for acute-phase diagnosis, detecting M. pneumoniae DNA/RNA with high sensitivity (90-95%) and specificity. Real-time PCR allows rapid results (2-4 hours) and can quantify bacterial load. Multiplex PCR panels simultaneously identify co-infecting pathogens, enhancing diagnostic efficiency.
Serological Antibody Testing
IgM/IgG detection remains widely used but has limitations. IgM appears 7-10 days post-infection, making it unreliable for early diagnosis. Paired acute/convalescent sera (4-week interval) improve accuracy but delay confirmation. ELISA and particle agglutination assays are common formats.
Rapid Antigen Detection
Lateral flow assays detecting M. pneumoniae antigens provide results in 15-30 minutes but suffer from lower sensitivity (60-70%). Useful as point-of-care screening in resource-limited settings, though negative results require PCR confirmation.
Culture Isolation
Though historically the diagnostic standard, culture requires specialized media (SP4) and takes 2-6 weeks, with sensitivity below 60%. Mainly used for research and antimicrobial susceptibility testing due to its impracticality in clinical practice.
Emerging Detection Methods for Mycoplasma Pneumoniae Infection
Traditional methods face limitations such as low sensitivity, slow turnaround time, and technical complexity. Emerging detection technologies are revolutionizing the field of M. pneumoniae diagnostics by providing faster, more accurate, and more convenient solutions, enabling timely diagnosis and improved clinical management.
- Nanostructured Electrode Biosensor: Enzyme-free detection using methylene blue hybridization; enhances gene differentiation by 3.5-fold.
- Silver Nanorod SERS Platform: Raman spectroscopy-based ultrasensitive detection; effective for clinical throat swab samples.
- Recombinase-Aided Amplification (RAA): Rapid isothermal (39°C) nucleic acid amplification; 15-30 minutes detection with perfect accuracy.
- Multicross Displacement Amplification (MCDA) + Lateral Flow Biosensor: Combines DNA amplification with nanoparticle detection; enables point-of-care testing in resource-limited settings.
Conclusion
The advancement of emerging diagnostic technologies for Mycoplasma pneumoniae marks a transformative shift from traditional, time-consuming methods to rapid, precise, and accessible solutions. These innovations, from nanostructured biosensors to isothermal amplification, address critical challenges in pediatric and clinical settings, enabling timely diagnosis and targeted treatment.
Alta DiagnoTech provides a comprehensive suite of IVD solutions for Mycoplasma pneumoniae diagnostics, including real-time PCR kits, isothermal amplification systems and lateral flow rapid tests, delivering high-accuracy, rapid, and customizable diagnostic solutions for diverse healthcare settings. If you have related needs, please feel free to contact us for more information or product support.
Reference
- Tahmasebi, Hamed, et al. "Reemergence of Mycoplasma pneumoniae disease: pathogenesis and new approaches." Microbial pathogenesis 196 (2024): 106944.
This article is for research use only. Do not use in any diagnostic or therapeutic application.



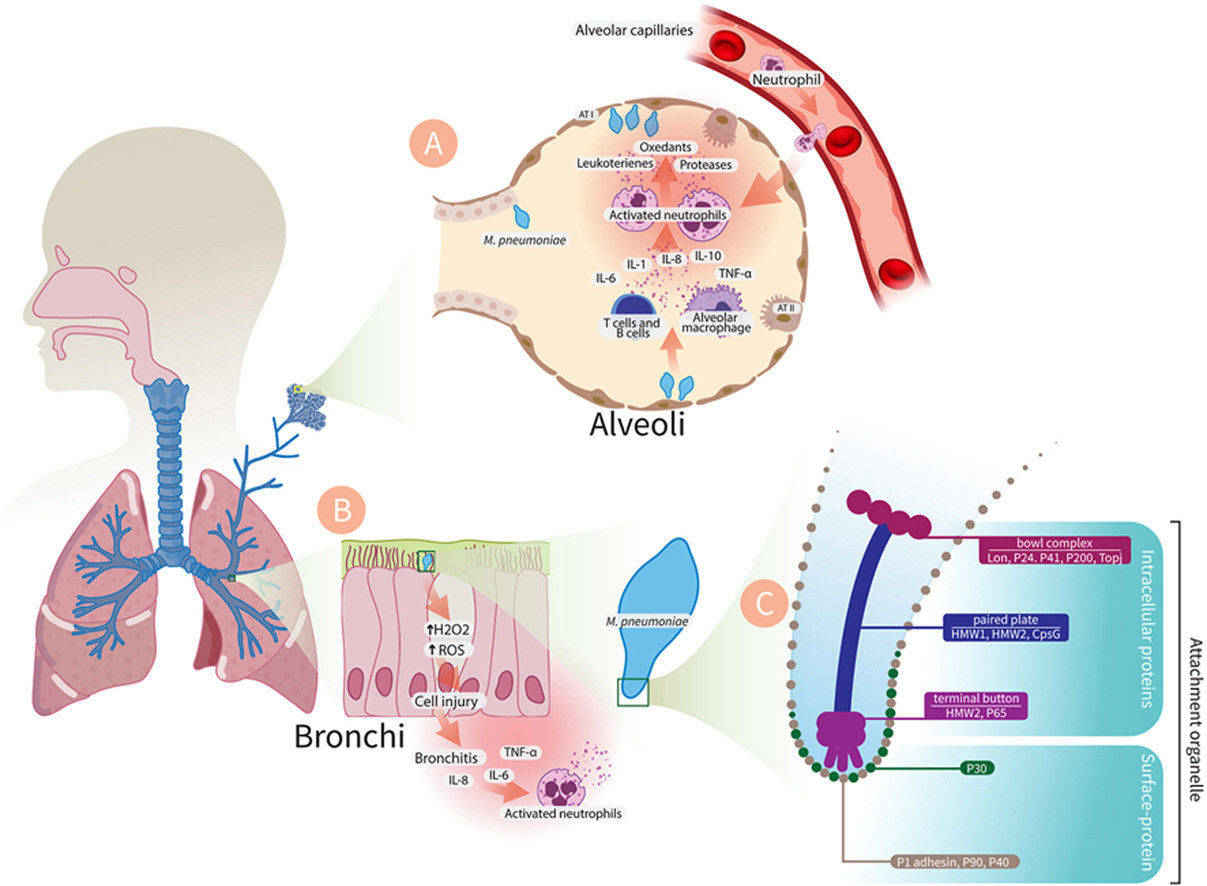 Fig.1 Pathogenesis of Mycoplasma pneumoniae infection. (Tahmasebi, Hamed, et al., 2024)
Fig.1 Pathogenesis of Mycoplasma pneumoniae infection. (Tahmasebi, Hamed, et al., 2024)



