Ureaplasma urealyticum is a clinically important yet often underdiagnosed pathogen that presents unique challenges in genitourinary and reproductive health management. This resource provides a comprehensive overview of modern diagnostic approaches, from clinical suspicion and traditional diagnostic methods to next-generation diagnostic solutions, providing healthcare professionals with evidence-based strategies for accurate detection and effective clinical decision-making.
Introduction to Ureaplasma Urealyticum Infection
Ureaplasma urealyticum is a clinically important yet often overlooked sexually transmitted pathogen associated with urogenital infections (e.g., non-gonococcal urethritis, prostatitis) and adverse pregnancy outcomes (e.g., preterm birth, chorioamnionitis). As one of the smallest free-living bacteria, its detection challenges include asymptomatic carriage, demanding growth requirements, and increasing antimicrobial resistance, highlighting the urgent need for advanced diagnostic solutions.
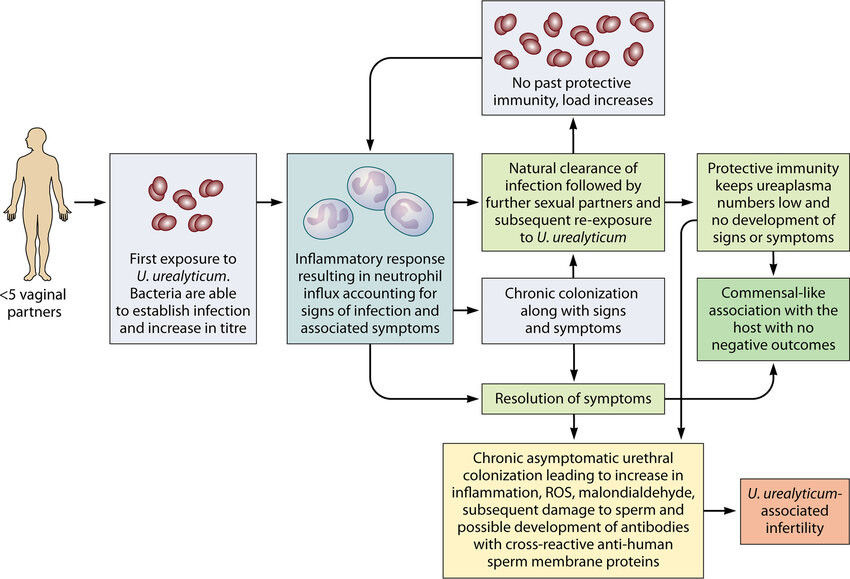 Fig.1 Proposed natural history of U. urealyticum urethral infection in men following initial exposure. (Beeton, Michael L., et al., 2019)
Fig.1 Proposed natural history of U. urealyticum urethral infection in men following initial exposure. (Beeton, Michael L., et al., 2019)
Clinical Diagnosis of Ureaplasma Urealyticum Infection
Ureaplasma urealyticum infections present diagnostic challenges due to their frequent asymptomatic carriage, nonspecific symptoms, and overlap with other urogenital pathogens. Clinical suspicion is often triggered by persistent or recurrent conditions, but laboratory confirmation is essential due to the lack of pathognomonic features.
- Symptomatic Presentations
Ureaplasma urealyticum testing is clinically indicated for persistent/recurrent urogenital inflammation unresponsive to first-line therapies, including: nongonococcal urethritis (NGU) with lingering discharge/dysuria, chronic prostatitis or pelvic pain, and suspected pelvic inflammatory disease (PID) with negative routine STI screens. Testing is also critical for adverse pregnancy outcomes (e.g., preterm labor) and unexplained infertility (abnormal semen parameters or endometritis) when other causes are excluded.
- High-Risk Populations (Asymptomatic)
Asymptomatic screening should be considered for: individuals with recurrent pregnancy loss (due to placental colonization risks), couples undergoing fertility treatments, immunocompromised patients, neonates with sepsis/pneumonia (vertical transmission risk), and sexual partners of positive cases to break reinfection cycles.
Traditional Methods for Ureaplasma Urealyticum Diagnostics
Traditional diagnostic approaches for Ureaplasma urealyticum have significant limitations but remain historically important. The primary methods include:
Culture-Based Detection
The traditional gold standard involves culturing Ureaplasma urealyticum in specialized media (e.g., A8 broth or U9 agar), which detect urease activity through pH changes. However, this method is slow (2–5 days), has low sensitivity (60–70%), and cannot differentiate U. urealyticum from U. parvum without further testing.
Serology (Antibody Detection)
Serological tests (e.g., ELISA) measure antibodies but are rarely used clinically due to cross-reactivity with other Mycoplasma species and poor correlation between antibody levels and active infection. Asymptomatic carriers may test positive, limiting diagnostic utility.
Microscopy & Biochemical Tests
Direct staining (e.g., Giemsa) lacks specificity, while urease activity tests provide only presumptive results. These methods are largely obsolete due to their inability to reliably confirm U. urealyticum infection compared to modern molecular techniques.
Next-generation Solutions for Ureaplasma Urealyticum Diagnostics
The limitations of traditional diagnostic methods for Ureaplasma urealyticum have driven the development of advanced, rapid, and highly accurate detection technologies. These next-generation solutions address critical challenges such as low sensitivity, slow turnaround times, and the inability to assess antimicrobial resistance (AMR).
Molecular Diagnostics (PCR & qPCR)
PCR and qPCR are now the gold standard for Ureaplasma urealyticum detection, offering >95% sensitivity/specificity with results in 2-4 hours. qPCR additionally quantifies bacterial load, while multiplex panels simultaneously detect co-infecting STIs like Chlamydia and Mycoplasma genitalium.
Isothermal Amplification (RPA, LAMP, MCDA)
These portable alternatives to PCR amplify DNA at constant temperatures, enabling rapid (<30 min), equipment-free testing ideal for clinics. LAMP provides visual color-change results, while RPA's extreme sensitivity makes it valuable for low-resource settings.
Antimicrobial Resistance (AMR) Profiling
Direct detection of resistance genes (ermB, tetM) from clinical samples guides antibiotic selection, particularly crucial given rising macrolide resistance (up to 50-80% in some regions). This prevents treatment failures in persistent infections.
Next- generation Sequencing (NGS) & Metagenomics
NGS provides comprehensive analysis of urogenital microbiota, identifying U. urealyticum alongside other pathogens and novel resistance markers. Particularly valuable for complex, recurrent infections and research applications.
Future of Ureaplasma Urealyticum Diagnostics
The future of Ureaplasma urealyticum diagnostics lies in rapid, precise, and accessible technologies, including point-of-care tests for equipment-free detection, AI-powered analysis of metagenomic data for comprehensive microbiome profiling, and microfluidic chips integrating multiplex PCR with AMR marker detection. All aimed at overcoming current limitations in sensitivity, speed, and resistance monitoring to enable personalized treatment and global surveillance.
Alta DiagnoTech provides comprehensive IVD products for Ureaplasma urealyticum detection, offering advanced PCR kits and rapid isothermal testing platforms to ensure accurate diagnosis and targeted treatment. If you have related needs, please feel free to contact us for more information or product support.
Reference
- Beeton, Michael L., Matthew S. Payne, and Lucy Jones. "The role of Ureaplasma spp. in the development of nongonococcal urethritis and infertility among men." Clinical microbiology reviews 32.4 (2019): 10-1128.
This article is for research use only. Do not use in any diagnostic or therapeutic application.



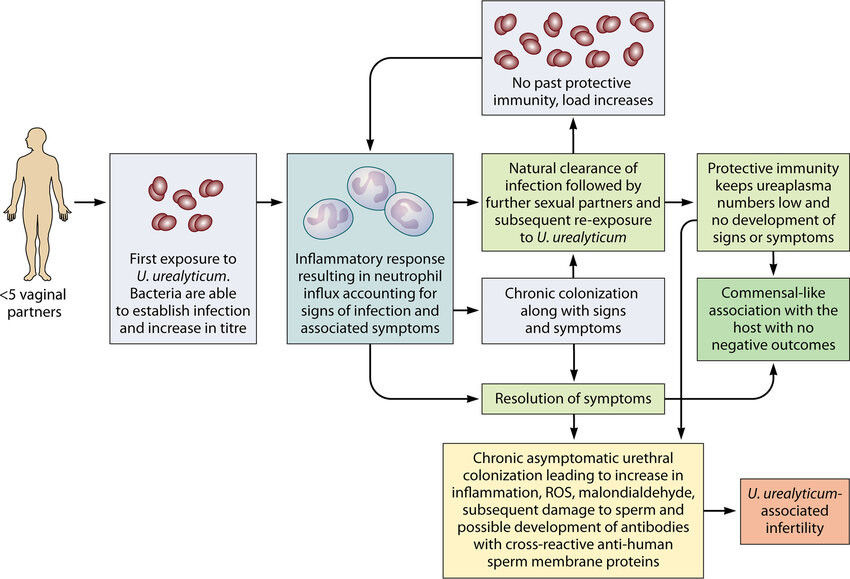 Fig.1 Proposed natural history of U. urealyticum urethral infection in men following initial exposure. (Beeton, Michael L., et al., 2019)
Fig.1 Proposed natural history of U. urealyticum urethral infection in men following initial exposure. (Beeton, Michael L., et al., 2019)





